Annual Breast Cancer Screening from Age 40-79 Offers Highest Mortality Reduction

Published in Radiology, New Research Challenges Existing Screening Recommendations
In a breakthrough study published in the Radiological Society of North America (RSNA), researchers have shed new light on breast cancer screening practices. The study, led by Dr. Debra L. Monticciolo, has revealed compelling evidence in favor of annual breast cancer screening beginning at age 40 and continuing through at least age 79.
Breast cancer remains a significant health concern for women in the United States. Ranking as the second most common cause of cancer death. Despite the well-documented effectiveness of regular screening mammography in reducing breast cancer mortality by 40%. A staggering percentage of eligible women—only 50% or less—actually participate in annual screening.
Debates Over Screening Recommendations
Dr. Monticciolo noted the ongoing debate surrounding breast cancer screening recommendations, particularly regarding the age at which to commence screening and its frequency. The 2009 recommendation by the U.S. Preventive Services Task Force (USPSTF) advocating for biennial screening starting at age 50 resulted in a decline in screening participation nationwide. However, the USPSTF revised its stance in 2023, suggesting biennial screening between ages 40 and 74. In contrast, organizations such as the American College of Radiology, the Society of Breast Imaging, and the National Comprehensive Cancer Network endorse annual screening for women at average risk beginning at age 40.
Study Methodology and Analysis
The study conducted by Dr. Monticciolo and her team involved a secondary analysis of Cancer Intervention and Surveillance Modeling Network (CISNET) 2023 median estimates of breast cancer screening outcomes. CISNET modeling provided the opportunity to estimate screening outcomes at various frequencies and starting ages using U.S. data.
Comparing four different screening scenarios—biennial screening of women aged 50-74, biennial screening of women aged 40-74, annual screening of women aged 40-74, and annual screening of women aged 40-79. The researchers found that annual screening of women aged 40-79 resulted in the highest mortality reduction at 41.7%. Additionally, this approach showed the lowest per mammogram false-positive screens (6.5%) and benign biopsies (0.88%) compared to other scenarios.
Implications and Recommendations
Dr. Monticciolo emphasized the importance of their findings, stating that annual screening from age 40 to 79 provides the highest mortality reduction, most cancer deaths averted, and most years of life gained. She highlighted the manageable nature of screening risks compared to the potential lethality of advanced breast cancer.
The USPSTF’s concerns include recall rates and benign biopsies as potential harms. Dr. Monticciolo underscored the manageable nature of these risks compared to the benefits of early cancer detection. She urged primary care physicians to recognize the tremendous benefits of annual screening for women aged 40. Additionally, emphasized the need to prioritize women’s lives by adopting early detection strategies.
The study adds to the growing body of evidence supporting annual screening from age 40. Breast cancer being easier to treat when detected early. The findings underscore the importance of regular screening in saving lives and reducing the burden of advanced-stage disease.
Dr. Monticciolo expressed hope that the study’s findings would encourage policymakers to prioritize annual screening from age 40. Thus ensuring that more women have access to life-saving early detection measures.
Stay informed and engaged with the latest advancements. Empower yourself with knowledge and make more informed decisions about your breast cancer treatment and care. Visit the Breast Advocate App website today and join us in the fight against breast cancer.
Does MS Affect Breast Cancer Diagnosis and Screening?
According to a new study published in the online issue of Neurology®, women with multiple sclerosis (MS) are less likely to have breast cancers detected through routine cancer screenings than women without MS.
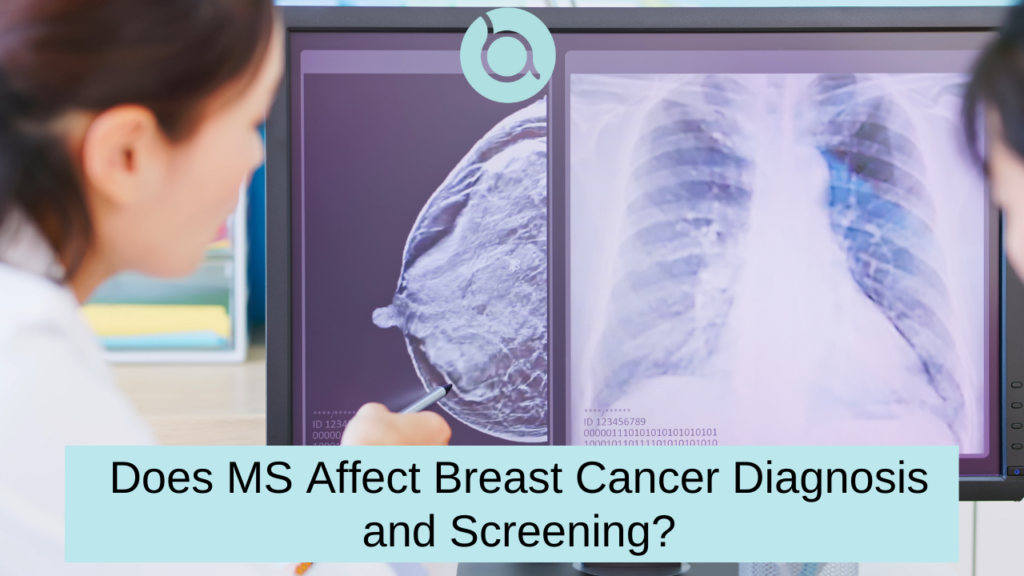
According to a new study published in the online issue of Neurology®, women with multiple sclerosis (MS) are less likely to have breast cancers detected through routine cancer screenings than women without MS.
Researchers looked at health care data for 14.8 million people in Ontario to see if there were any individuals diagnosed with breast or colorectal cancer who also had MS. For the study, they compared 351 women with breast cancer and MS to 1,404 women with breast cancer but no MS. They also identified 54 people with colorectal cancer and MS, and compared these to 216 people with colorectal cancer and no MS.
The team discovered that routine screening revealed breast cancer in 103 (29%) of the women with MS, and in 529 (38%) of the women without MS. After controlling for age, diagnosis year, and income, they found women with MS had a 32% decreased chance of having breast cancer diagnosed through routine screening.
“Disability from MS increases with age, as does cancer risk, so it is likely that those with MS may find it more difficult to get regular mammograms as they get older,” said study author Ruth Ann Marrie, MD.
Researchers also discovered that 21% of people with MS and breast cancer, and 33% of those with MS and colorectal cancer, had a level of impairment that required long-term care. “More research is needed regarding the role of MS-related disability on screenings,” states Marrie.
One limitation was the study did not include the time period from when a person first noticed cancer symptoms to when they told their doctor. “People experiencing marginalization due to race or ethnicity have different access to cancer screening, and this may be exacerbated among people with MS,” said Marrie. She stated that race and ethnicity data were not accessible for this study and that future research should look into it.
General Breast Cancer Screening Guidelines
Regular screenings can help find cancers earlier before they have a chance to spread. Below are the American Cancer Society’s recommendations on breast cancer screening:
- Women ages 40 to 44: If they choose, they should start annual breast cancer screening early with mammograms.
- Women ages 45 to 54: Should get mammograms every year.
- Women ages 55 and older: Should get mammograms every 2 years, however, annual screening can be continued.
Breast Cancer – What Symptoms Should I Take Seriously?
According to the CDC, some of the warning signs of breast cancer include:
- New lump in the breast or underarm (armpit).
- Thickening or swelling of part of the breast.
- Irritation or dimpling of breast skin.
- Redness or flaky skin in the nipple area or the breast.
- Pulling in of the nipple (known as “nipple retraction”), or pain in the nipple area.
- Nipple discharge other than breast milk, including a bloody discharge.
- Any change in the size or the shape of the breast.
- Pain in any area of the breast.
If you notice any of these symptoms or something else that concerns you, schedule an appointment with your doctor right away.
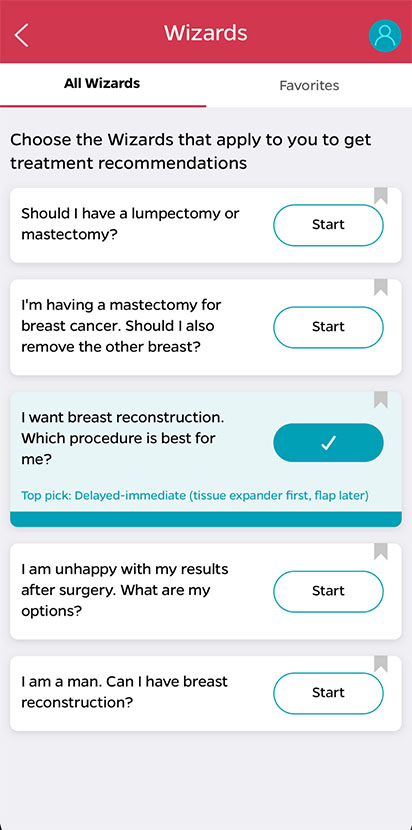
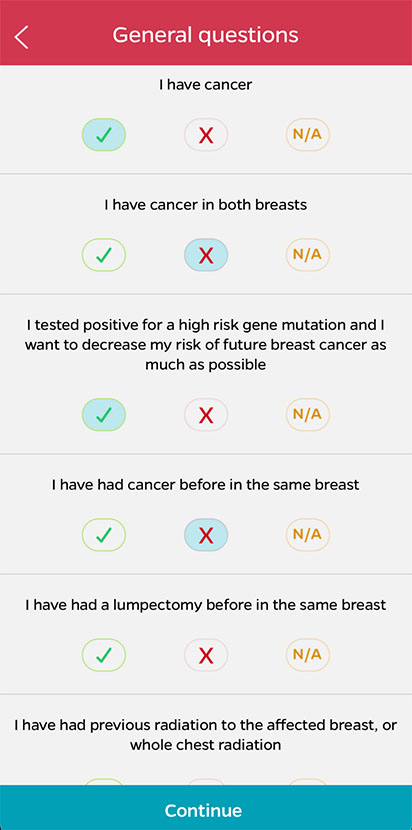
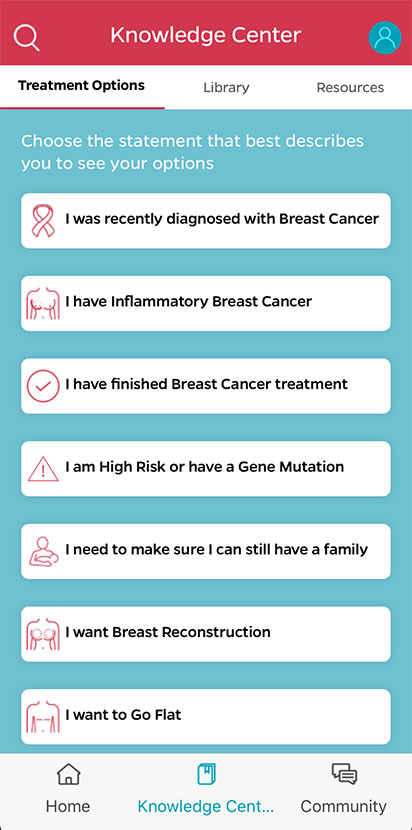
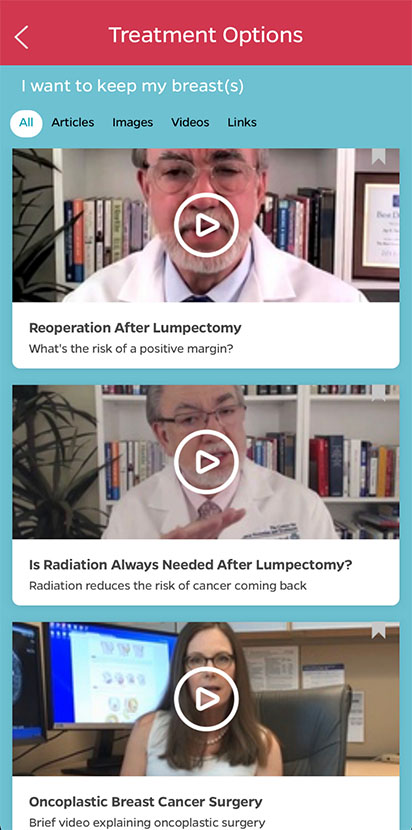
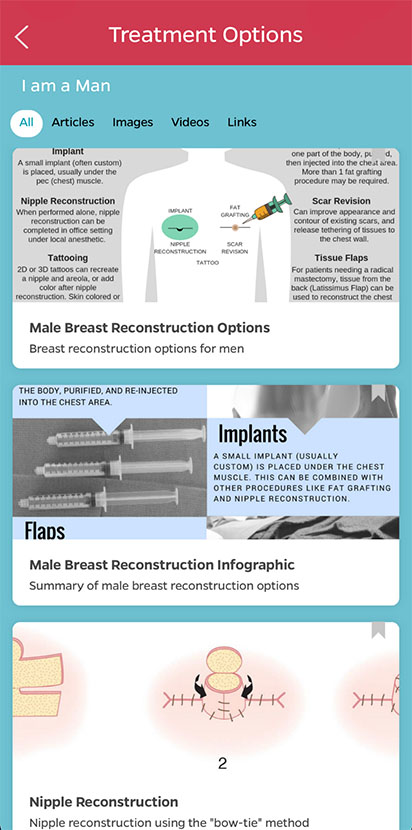
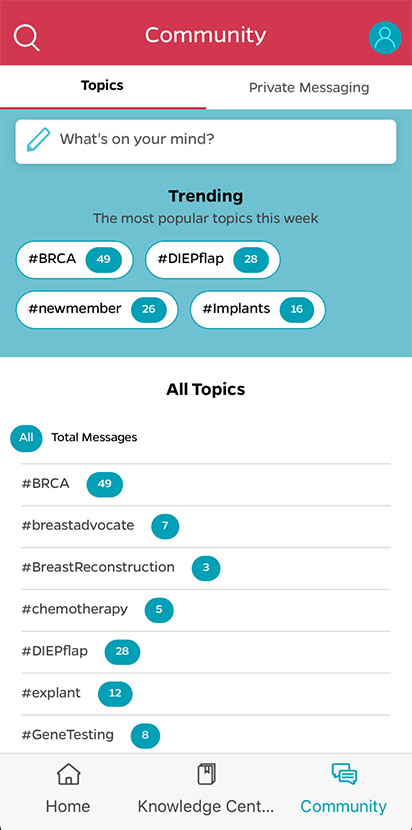
If you are facing surgery for breast cancer, or are considering surgery to decrease your risk of developing breast cancer – Breast Advocate® is for you.
Should Breast Cancer Screening for Black Women Start Sooner?

Breast cancer is still the most prevalent cancer diagnosed in women in the United States and the second greatest cause of cancer mortality. According to the American Cancer Society, more than 281,550 new cases of invasive breast cancer and 49,290 new cases of non-invasive breast cancer will be diagnosed this year.
Recent data published by the American Cancer Society shows black women have a 40% higher death rate from breast cancer than white women. The disparity is even greater among women under the age of 50: the death rate among young black women is double that of young white women. Unfortunately, advancements in treatment have not benefited all groups equally.
What Causes the Disparity in Breast Cancer Rates Among Black Women?
Research shows the reasons for the disparity in breast cancer outcomes is complex. Disparities may be explained in part by social, economic, and behavioral factors. Diabetes, heart disease, and obesity are more common among black women, all of which are risk factors for breast cancer. It is becoming more obvious that tumor biology also plays a role. Triple-negative breast cancer and inflammatory breast cancer strike black women disproportionately, and they are more likely to be detected at younger ages and at later stages of the illness.
“It is widely known in the medical community that BRCA1 and BRCA2 mutations are prevalence in the Jewish community, but what is not widely known is that they are also prevalent in Black women,” shares Debra Monticciolo, vice-chair of the department of radiology and chief of breast imaging at Baylor Scott and White Medical Center. “We also know that Black women have higher death rates and these women have a twofold increased risk for triple-negative breast cancer.”
What’s the Solution?
According to research published in Annals of Internal Medicine, biannual mammography screening starting at the age of 40 might lower breast cancer-related mortality among black women by 15%.
“Minority women should begin screening for breast cancer at age 40 years instead of age 45 or 50 years, as they are 72% more likely to be diagnosed with invasive breast cancer younger than the age of 50 years, 58% more likely to have advanced breast cancer at presentation younger than age 50 years, and 127% more likely to die younger than age 50 years compared with white women. We are failing Black women,” continues Monticciolo.
Women with greater resources (such as higher levels of education and wealth) may be better able to take advantage of healthcare breakthroughs. Cities that have tackled this issue by expanding access to state-of-the-art mammography facilities have shown great success in closing the breast cancer mortality disparity between black and white women.
Screening Mammograms Shown to Reduce Deaths Caused by Advanced Breast Cancer
There is a constant debate on whether screening mammograms offer a significant benefit to patients.

In the American Cancer Society journal, CANCER, a Swedish study has found that early mammogram screenings can significantly reduce the number of deaths from metastatic breast cancer.
The study evaluated 549,091 women, covering approximately 30% of the screening‐eligible population in Sweden. The results showed that women who had regular screening mammograms had a statistically significant 41% reduction in their risk of dying of breast cancer within 10 years, and a 25% reduction in the rate of advanced breast cancers, compared to individuals who did not participate in mammogram screenings. According to the study, these benefits appeared to be independent of recent changes in patient treatment regimens.
The study concludes that the “benefits of participating in mammography screening are truly substantial and save lives through early detection, lives that otherwise would have been lost under the prevailing therapy at the time of diagnosis.”
This study offers encouraging insight into the benefits of regular breast cancer screening. It is important for both women and men to discuss their overall risk of developing breast cancer to determine the best time to begin screening, and how often they should be screened.
Performing monthly at-home self-breast exams is also a very important, free screening tool everyone should practice in addition to regular radiologic screening. However, this should not replace the imaging screening recommended by your healthcare team.
If access to care or cost is keeping you from following through with your recommended breast cancer screening appointment, please check out the Financial Assistance tab within the Resource section in the Breast Advocate app.
Supplemental MRI Screening May Benefit Women with Extremely Dense Breast Tissue
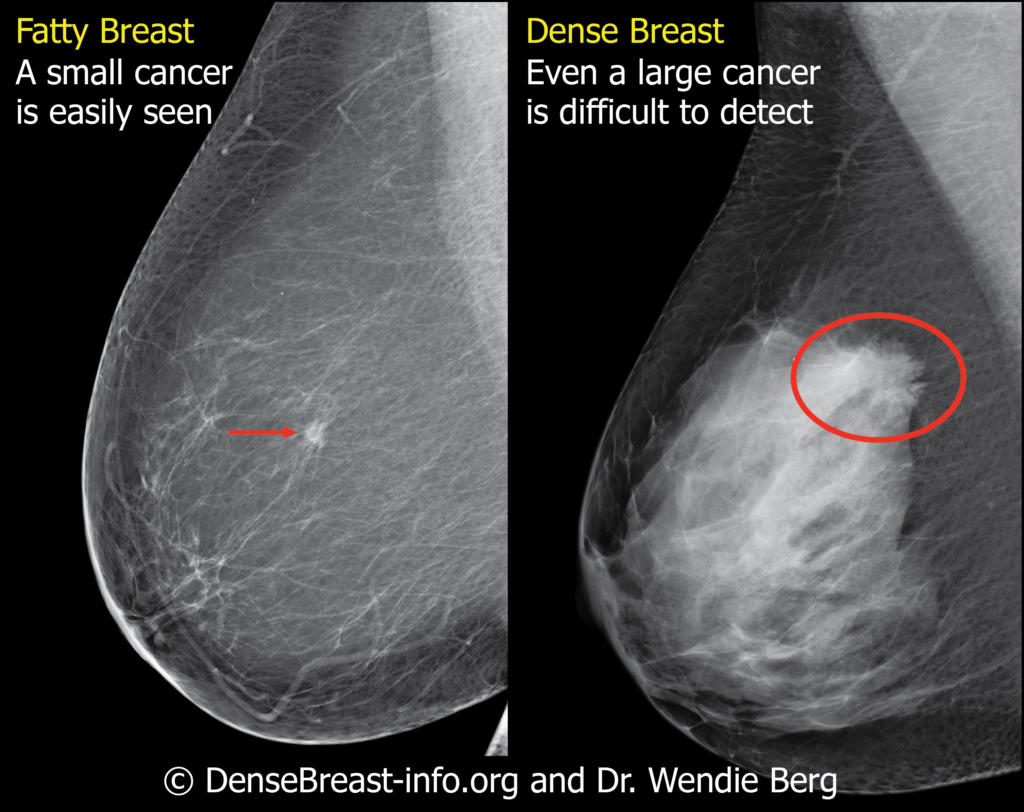
Women with extremely dense breast tissue have a 4 to 6 times increased risk of developing breast cancer, and their cancers are also less likely to be detected on a mammogram. About 50% of women have dense breasts.
New laws in many US states were recently passed requiring mammogram reports to include information on the density of a woman’s breast tissue. Dense breast tissue is a risk factor for breast cancer and can make detecting breast cancer more difficult with screening mammograms alone. For this reason, more research is underway to determine how to best screen for cancer in women with dense breasts.
So what are “dense breasts”? Breasts consist of fibrous glandular tissue and fat. Dense breasts contain more fibrous tissue and less fat. On a mammogram, dense fibrous tissue has the same white appearance as a breast cancer. This can make it very difficult for radiologists to spot the breast cancer.
A long-standing question is whether or not women with dense breasts should undergo additional imaging screening tests in combination with mammograms. A new study published in the New England Journal of Medicine offers new insight supporting the addition of MRI screening to mammograms for women with extremely dense breast tissue.
The study was conducted in the Netherlands. 40,373 women between the ages of 50 and 75 years with extremely dense breasts and normal screening mammograms were randomized to undergo additional screening via MRI, or receive no additional screening. The study results showed the mammogram plus MRI group experienced 50% fewer interval cancers than the mammogram-only group during a 2-year period (2.5 vs 5 per 1,000 screenings, respectively). The tumors detected on MRI were smaller, of an earlier stage, and more likely to be node-negative than those detected in the mammography-only group.
This study suggests that a combination of mammograms and MRIs can be beneficial for women with extremely dense breast tissue in detecting breast cancer at an earlier stage than mammograms alone. However, it is important to note the results of this study do not suggest adding MRIs will decrease the death rates from breast cancer.
It is important to discuss your screening options with your health care team to see if additional MRI imaging would be beneficial for you based on your specific situation and risk of developing breast cancer.
Rising Breast Cancer Rates Among Younger Women in Canada Highlight Urgent Need for Awareness

Increasing breast cancer rates among women in Canada
A recent study led by Dr. Jean Seely, published in the Canadian Association of Radiologists Journal. The study highlights a concerning increase in breast cancer rates among Canadian women under 50. The study observed a increasing breast cancer rates among women in Canada in their twenties, thirties, and forties over the past 35 years. Calling for urgent action to address the trends.
Dr. Seely serves as the Head of Breast Imaging at The Ottawa Hospital and is a Professor in the Department of Radiology at the University of Ottawa. She led the team analyzing historical data from the National Cancer Incidence Reporting System (1984-1991) and the Canadian Cancer Registry (1992-2019). They reviewed all breast cancer diagnoses among women aged 20 to 54, revealing a significant increase in rates.
- Twenties: From 3.9 cases per 100,000 between 1984 and 1988. To 5.7 cases per 100,000 between 2015 and 2019, marking a 45.5% increase.
- Thirties: From 37.7 cases per 100,000 between 1984 and 1988. To 42.4 cases per 100,000 between 2015 and 2019, a 12.5% rise.
- Forties: From 127.8 cases per 100,000 between 1984 and 1988. To 139.4 cases per 100,000 between 2015 and 2019, a 9.1% increase.
“Breast cancer in younger women tends to be diagnosed at later stages and is often more aggressive,” Dr. Seely noted. “It’s alarming to see rising rates among women in their twenties and thirties.”
Dr. Seely, and Dr. Anna Wilkinson, emphasized that younger women must be included in awareness campaigns and screening programs. Traditionally, public health efforts have targeted women over 50. The rising incidence in younger groups demands a re-evaluation of strategies.
Personal Impact
Chelsea Bland, one of the women impacted, shared her experience. After hearing of a death from breast cancer at age 33, she self-examined at 28 and discovered a lump. This led to her diagnosis, treatment, and now being two years cancer-free. Bland’s experience propelled her to co-found a support group for younger women, aged 28 to 40.
“I hope […] people will rethink saying that being in your twenties, thirties, and forties is too young for breast cancer,” she shared. “In my support group, I have heard the same story repeatedly. Young women aren’t being taken seriously after finding a lump because they’re told they’re too young for breast cancer.”
Next Steps
The research team called for further investigation into the root causes of this increase. Such findings could inform new, more targeted intervention strategies.
“We’re calling for increased awareness among healthcare professionals and the public regarding the rising incidence of breast cancer in younger women,” emphasized Dr. Seely. “We must adapt our strategies and policies to reflect these changing trends, ensuring that all women, regardless of age, have access to the information and resources they need to detect and combat this disease.”
These findings underscore the urgent need for greater awareness, research, and proactive healthcare policies. Addressing the evolving landscape of breast cancer among younger women in Canada.
Stay informed and engaged with the latest advancements. Empower yourself with knowledge and make more informed decisions about your breast cancer treatment and care. Visit the Breast Advocate App website today and join us in the fight against breast cancer.
Breakthrough in Breast Cancer Prevention: Scientists Target Cells-of-Origin in BRCA2 Carriers

Unveiling the Source of Cancer in High-Risk Individuals
In a landmark study led by the Walter and Eliza Hall Institute of Medical Research (WEHI) in Australia, scientists have made a significant breakthrough in the fight against BRCA2 gene breast cancer. The research, recently published in Nature Cell Biology, identifies for the first time the likely ‘cells-of-origin’. The specific cells that can develop into breast cancer in individuals carrying this genetic mutation.
Women inheriting the faulty BRCA2 gene face a daunting approximately 70% lifetime risk of developing breast cancer. Often at a younger age and with a tendency towards clinical aggression. Preventive strategies have thus far been limited to early screening and preventive surgeries, such as mastectomies, to lower this risk.
A Targeted Approach to Cancer Prevention
The study’s co-first author, Dr. Rachel Joyce, highlighted the discovery of an aberrant cell population within the breast tissue of BRCA2 carriers. These cells, identified in the majority of healthy tissue samples from carriers, divide more rapidly than normal. Thus suggesting their pivotal role as the originators of potential future breast cancers in these women.
Further insights from the study revealed these aberrant cells to be a subset of luminal progenitor cells in breast ductal tissues. Displaying altered protein production – a key factor in tissue growth and function. This alteration not only earmarks these cells as the likely origin of cancer. But also exposes a vulnerability to existing cancer treatments.
Towards a New Era of Prevention
Leading the research, Professor Jane Visvader and her team developed a pre-clinical BRCA2 model demonstrating similar alterations. They targeted these cells with Everolimus, an approved drug for relapsed breast cancer, showing that pre-treatment could delay tumor formation. This finding opens new avenues for preventive treatment strategies, aiming at specific aspects of protein production in these cells.
Despite the promising outcomes, the journey from lab to clinic remains cautious. Professor Geoff Lindeman, a study author and cancer clinician, emphasized the need for further research to refine these approaches, considering the potential side effects of drugs like Everolimus when used as preventive treatments. The goal is to develop more selective and tolerable treatments for BRCA2 mutation carriers, building on the significant strides already made in identifying the cells-of-origin for breast cancer linked to the BRCA1 gene mutation.
The study, supported by contributions from the Victorian Cancer Biobank, the National Health and Medical Research Council, and several other foundations, marks a critical step forward in the quest for effective breast cancer prevention strategies. It not only sheds light on the cellular beginnings of breast cancer in high-risk groups but also charts a course towards potentially life-saving treatments for women worldwide.
Stay informed and engaged with the latest advancements. Empower yourself with knowledge and make more informed decisions about your breast cancer treatment and care. Visit the Breast Advocate App website today and join us in the fight against breast cancer.
New Research Offers Hope for Breast Cancer Patients – Mortality Rates Show Steady Decline

A recent population-based study provides valuable insights into long-term breast cancer mortality rates. The research sheds light on the improving prognosis for breast cancer survivors. Advancements in treatment and care have led to increasingly better outcomes over the years.
Favorable Trend in Mortality Rates
The study analyzed data from women in England diagnosed with early invasive breast cancer between 1993 and 2015. The annual breast cancer mortality rate was the highest during the five years following diagnosis. After that, mortality showed a steady decline.
Researchers further delved into each calendar period of diagnosis 1993-1999, 2000-2004, 2005-2009, and 2010-2015. The annual breast cancer mortality rates decreased with each successive calendar period. This indicates a clear trend of improvement in breast cancer management and treatment, leading to higher chances of survival for patients diagnosed with breast cancer.
Decline in Five-Year Mortality Risk
A key finding from the study is the significant decrease in the five-year breast cancer mortality risk over time. For women diagnosed between 1993-1999, the risk was 14.4%. For those diagnosed between 2010-2015, the risk dropped significantly to 4.9%.
The researchers also considered various patient and tumor characteristics among women diagnosed in 2010-2015. They discovered that the cumulative five-year breast cancer mortality risk varied substantially based on these factors. Overall, the 5 year risk of death from breast cancer in patients with a recent diagnosis was under 3% for 62.8% of women. However, the risk remained 20% or higher for 4.6% of women.
Study Take-Aways
This study shows the substantial improvement in prognosis for women with a diagnosis of early invasive breast cancer that has been made since the 1990s. Advancements in treatment modalities are having a favorable impact.
These findings will reassure most women treated for early stage breast cancer that they are likely to become long term survivors. They can also be used to identify and further study the groups of women for whom the risk of breast cancer mortality remains substantial.
Early Detection Remains Crucial
The great news is that the overall outlook for breast cancer outcomes continues to improve. However, this study also underscores the importance of early detection to ensure diagnosis occurs at the earliest stage possible.
Encouraging Rise in Breast Cancer Survival Rates
A recent study published in Nature shows breast cancer survival rates have improved significantly over the past few decades. Women diagnosed since 2010 have a much lower risk of dying than those diagnosed in the 1990s. Thanks to advancements in medical research, improved screening methods, and more effective treatments, patients now have a significantly higher chance of surviving after a breast cancer diagnosis. Research shows that the number of women who die from their disease has decreased by two-thirds. This progress represents a transformative shift in the work against breast cancer, offering some hope and renewed optimism to patients and their loved ones.
Early Detection: The Power of Screening
One of the primary factors contributing to the increase in breast cancer survival rates is early detection. Regular mammograms and other screening methods allow the identification of breast cancer at its earliest stages, often before symptoms even arise. Early detection allows for prompt intervention and treatment, leading to higher survival rates.
Awareness campaigns and education initiatives also play a vital role in encouraging women to have regular screenings, leading to earlier diagnoses and improved outcomes. According to Naser Turabi, director of evidence and implementation at Cancer Research UK (CRUK) in London, the decline in the mortality rate wasn’t unexpected. “Research is incredibly important to determine the success of treatments,” he says, and this study will help people to make better-informed decisions about their treatment.
Advancements in Treatment: Targeted Therapies and Precision Medicine
Significant advancements in treatment options have revolutionized breast cancer care. Targeted therapies, such as hormone therapy, HER2-targeted therapy, and immunotherapy are designed to attack specific characteristics of cancer cells. This maximizes the effectiveness of the treatment while minimizing side effects. Additionally, chemotherapy regimens and radiation therapy have become more precise and tailored to individual patients. This limits damage to healthy cells as much as possible and improves overall treatment outcomes. Surgical techniques have also advanced, with improved breast-conserving surgeries and reconstructive options also available to patients.
Collaborative Efforts
The collaborative efforts of researchers, healthcare professionals, and patient advocacy organizations have further propelled progress in breast cancer survival rates. Increased funding for research has led to breakthrough discoveries in understanding the biology of breast cancer, allowing for the development of innovative treatments.
“Involving patients was crucial to the study,” according to Carolyn Taylor, lead author of the study and an oncologist at the University of Oxford, UK. To direct their research, the scientists appointed two patient representatives. “They looked at the analyses and gave comments and suggestions throughout the study. And they helped us to interpret the results in the way that patients can understand.”
Improved coordination and multidisciplinary approaches among healthcare teams have enhanced the quality of care provided to patients, ensuring that they receive comprehensive treatment plans tailored to their specific needs.
A Brighter Future
While there is still much work to be done, the significant increase in breast cancer survival rates represents a remarkable achievement in the field of oncology. It highlights the power of early detection, improved treatments, and the tireless dedication of researchers and healthcare professionals. As we continue to advance in our understanding of breast cancer and refine treatment approaches, there is hope for an even brighter future: a future where breast cancer becomes a manageable and survivable disease for all.
AI May More Accurately Predict Breast Cancer Risk
Early detection plays a crucial role in improving breast cancer survival rates and treatment outcomes. The integration of artificial intelligence (AI) into radiologic imaging, like mammograms and MRIs, is revolutionizing breast cancer diagnosis.
In a recent study, artificial intelligence (AI) outperformed the standard clinical model for predicting the five-year risk for developing breast cancer.
AI Study of Screening Mammograms
Lead investigator, Dr. Vignesh Arasu, used data from screening mammograms at Kaiser Permanente in Northern California in 2016 that showed no visible evidence of cancer. “We selected from the entire year of screening mammograms performed in 2016, so our study population is representative of communities in Northern California.”
Five different artificial intelligence (AI) algorithms were used to generate risk scores for developing breast cancer over the five-year period using the 2016 screening mammograms. The risk scores were then compared to the Breast Cancer Surveillance Consortium (BCSC) clinical risk score as well as to one another.
“All five AI algorithms performed better than the risk model for predicting breast cancer risk at 0 to 5 years,” Dr. Arasu said. “This strong predictive performance over the five-year period suggests AI is identifying both missed cancers and breast tissue features that help predict future cancer development. Something in mammograms allows us to track breast cancer risk. This is the ‘black box’ of AI.”
Advancements in AI for Breast Cancer Diagnosis
AI technology has made significant strides in recent years, bringing a paradigm shift in the field of breast cancer detection.
- Mammograms: AI-based systems can analyze mammographic images and assist radiologists in detecting early-stage abnormalities.
- Breast MRI: AI algorithms can analyze MRI images to identify suspicious areas, helping radiologists pinpoint potential cancerous lesions more accurately. By combining the power of AI with radiologic testing, medical professionals can achieve comprehensive and reliable breast cancer diagnosis.
Benefits of using AI
The integration of AI in breast cancer diagnosis offers numerous benefits:
- AI algorithms can assist in reducing false negatives and false positives, which are a persistent challenge in conventional mammography.
- AI can significantly enhance the efficiency and speed of breast cancer detection.
- AI can help bridge the expertise gap in breast cancer diagnosis.
Challenges and Ethical Considerations
While AI brings tremendous promise, it also raises important challenges and ethical considerations.
One critical challenge is the need for robust and diverse datasets to train AI algorithms effectively. Transparency and interpretability of AI algorithms are also crucial. Understanding the decision-making process of AI systems is vital for radiologists and patients to trust and validate the results.
We must also address issues surrounding patient privacy and data security. AI systems require access to extensive patient data, including medical records and imaging studies, which must be protected to safeguard patient confidentiality.
Striving for Better Patient Outcomes
AI algorithms can provide radiologists with powerful tools to improve accuracy, efficiency, and speed in diagnosing breast cancer lesions. By reducing false negatives and false positives, AI can also improve sensitivity and specificity, leading to better patient outcomes.