The Impact of COVID-19 on Breast Cancer Treatment
Published March 31, 2020. Updated April 10, 2020
Breast cancer does not take a break…even amid a global crisis like the Coronavirus pandemic. For most people, it’s already overwhelming to hear the words “you have breast cancer”. In the midst of the current COVID-19 outbreak, increased uncertainty and changes in treatment recommendations are elevating everyone’s anxiety further. Many people are now being told that their treatment plan is changing. If you’re one of them, please know that your breast cancer team is adjusting your treatment plan to keep you safe and limit your exposure to coronavirus. Breast cancer patients are at increased risk of severe symptoms if they get coronavirus. People with severe symptoms need admission to a hospital for supportive care and are more likely to need intensive care, ventilator support for severe breathing problems, and are also at increased risk of death.
A recent study published in the Lancet, a highly respected medical journal, evaluated 34 patients who were infected with Coronavirus but didn’t have any symptoms, and underwent elective surgery. All developed pneumonia and 20% died.
All the medical and surgical societies are prioritizing your safety during this pandemic. At the same time as maximizing your safety, your team won’t do anything that negatively impacts your long-term prognosis.
Individuals Needing Chemo and/or Radiation
Most facilities providing chemo and radiation therapy treatment for breast cancer patients remain open and necessary treatment is not being delayed. Vigilant cleaning, health screenings of all patients before they enter the facility, and the advisement of patients to wear masks are just a few of the many steps healthcare workers are implementing to ensure patient safety. In many places, patients are no longer allowed to bring someone with them during their chemo treatments.
Individuals Requiring Breast Cancer Surgery
COVID-19 is impacting the surgical plans of many patients. At this time, the White House and numerous surgical societies are issuing guidelines recommending all surgeries that are not immediately life-saving be postponed. The American College of Surgeons and the American Society of Breast Surgeons are recommending delaying any surgery where a 6-8 week delay would not impact clinical outcomes. This includes surgery for DCIS, stage one ER/PR+ invasive cancers, re-excisions, surgery for high-risk lesions, and prophylactic (risk-reducing) mastectomies. Wherever possible, patients are being treated with hormonal therapy (eg Tamoxifen), aromatase inhibitors, or neo-adjuvant chemotherapy to enable surgery to be delayed. Recommendations are also calling for scheduled mastectomies to be converted to lumpectomies when clinically acceptable. Patients still wanting a mastectomy (with or without reconstruction) will be able to return for their definitive surgery once the crisis has passed.
Individuals Choosing Breast Reconstruction
For patients wanting breast reconstruction, there will unfortunately be a delay between the lumpectomy/mastectomy and the reconstruction procedure in most situations. In the US, some institutions are still allowing tissue-expander reconstruction, but the American Society of Plastic Surgeons (ASPS) strongly advises all autologous (flap) reconstructions be delayed. Although breast reconstruction is considered medically necessary, it is not immediately life-saving. For many, delaying reconstruction is understandably devastating, but it is important to remember there is no deadline for reconstruction and your health and safety are the top priorities of your surgical team.
Although reconstructive surgeries around the globe are being postponed, patients can still use this waiting period to research all their reconstructive options to determine which procedure is best for them. The Breast Advocate app provides personalized evidence-based information and recommendations for breast cancer surgery and reconstruction, after taking your situation and personal preferences into account.
Individuals at High Risk
At this time, individuals interested in prophylactic (risk-reducing) surgery because they are at high risk for developing breast cancer (eg BRCA+), should continue to self-monitor for breast changes at home. All society guidelines are strongly urging all prophylactic surgeries be postponed. Screening mammograms and MRIs may be delayed in your location during this pandemic. If any concerning breast changes occur, call you healthcare provider for further diagnostic instructions. Please also talk to your physician about the option of taking tamoxifen to decrease your risk while you wait for surgery.
It is important to remember that we must all do our part to protect ourselves, our loved ones, and our healthcare providers during this overwhelming time. By taking these measures, your risk of contracting COVID-19 will be minimized, hospital admissions will be reduced, necessary PPE will be conserved for our healthcare providers on the front lines, and lives will be saved.
Coronavirus: What Breast Cancer Patients Need To Know
Originally published March 12, 2020. Updated May 2, 2020.
With the spread of Coronavirus increasing across the US and other countries, it is essential for breast cancer patients and individuals with underlying health conditions (eg heart, lung or kidney disease, diabetes, asthma) that compromise their immune system to be educated and proactive in taking steps to protect themselves from contracting this new disease. Breast cancer treatments like chemotherapy, targeted therapies, immunotherapy, and radiation make the immune system weaker. People who have weakened immune systems have a much higher risk of complications if they become infected with this virus. In addition to the common sense precautions we should all take to prevent infection, people who have recently completed or are still undergoing cancer treatment should be extra vigilant as they are at a higher risk of hospitalization, severe complications, and even death.
What is Coronavirus?

The coronaviruses are a family of viruses that cause illnesses ranging from the common cold to more serious respiratory diseases. Flu is caused by a different virus (influenza). There is no vaccine for this coronavirus yet and it will be several months before a vaccine is available.
The disease caused by Coronavirus, known as COVID-19, is a respiratory illness caused by a coronavirus previously only found in animals that was first identified in an outbreak in Wuhan, China, in December 2019. The disease is spread through mucus droplets from the nose or mouth that are released when an individual close to you coughs or sneezes. It is also possible that a carrier of the virus can infect others by simply exhaling close to them. The infection can also be spread by touching a surface that mucus droplets have landed on, and then touching your eyes, nose or mouth. Coronavirus can stay alive on surfaces outside the body for many days, depending on the surface (72 hrs – 5 days). The virus likes metal surfaces like door knobs, silverware and jewelry in particular (survives for 5 days).
It appears the Coronavirus is much more contagious than the Flu. People seem to be most contagious when they have symptoms, but you can also catch the virus from infected people who have no symptoms. At least 25% of people infected with Coronavirus won’t develop any symptoms at all, and can very easily unknowingly spread the virus. Those who do develop symptoms take on average 5 days to do so. For these reasons, Coronavirus is spreading much faster than the seasonal flu.
What are the symptoms of COVID-19?
Most people who become infected with coronavirus have mild respiratory symptoms, and some people will show no symptoms at all. However, symptoms can become severe in some people, and some have died from the illness.
Similar to symptoms associate with the flu or common cold, the most common symptoms of COVID-19 include fever, a dry cough and shortness of breath. The CDC recently added the following list of possible symptoms: chills, repeated shaking with chills, muscle pain, headache, sore throat, and new loss of taste or smell. Any of these symptoms can range from mild to severe.
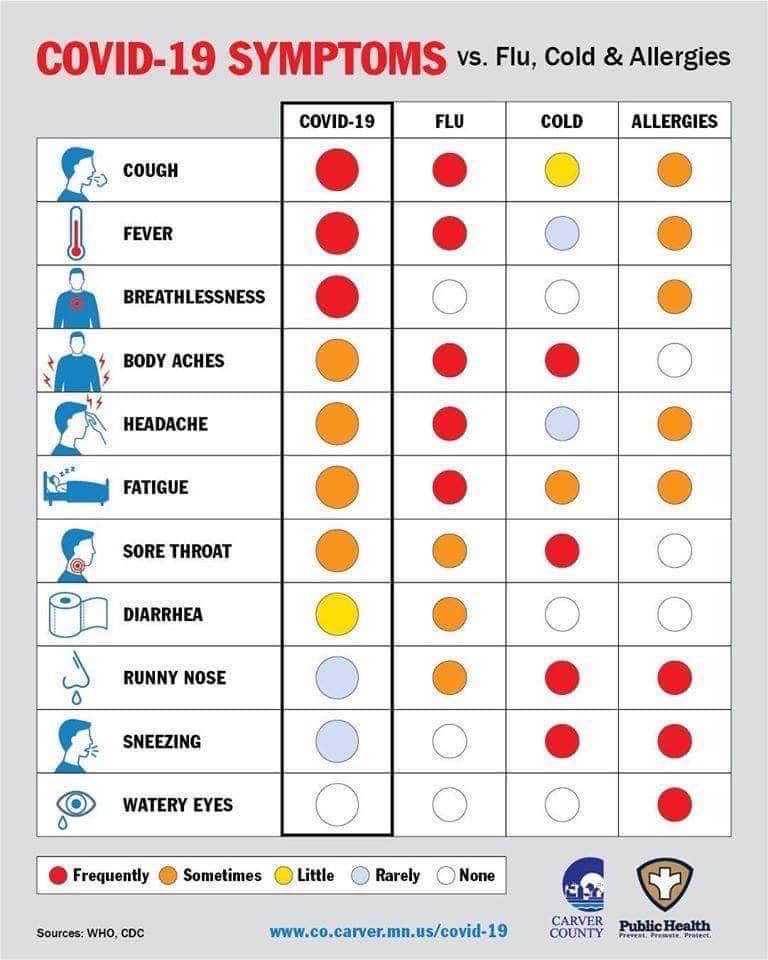
It is the impact on the lungs that doctors are most concerned about. According to the WHO, in people who have symptoms, about 40% will have mild symptoms, while 40% will develop mild to moderate pneumonia. About 15% of patients will need to be treated in hospital because of severe breathing difficulties. 5% will need the ICU and a ventilator. Patients who have recently completed or are undergoing cancer treatment are at higher risk of developing severe symptoms.
Based on the data available so far, the risk of death from COVID-19 in the general population is estimated by some models to be as high as 1%, which is 10x more fatal than the flu (about 0.1%). The real risk will only be known after widespread testing is available and we know how many people have been infected. Better knowledge of the disease process over time will likely also lead to improved, consistent treatment protocols that could also improve outcomes dramatically, and ultimately lower mortality to one that is more in line with the flu.
Most of the deaths have been in older patients with other medical conditions – the mortality rate for 60 – 64 year olds is about 4% for COVID-19. However, a significant number of younger people have also required admission to the hospital for supportive care. We are seeing deaths in all age groups, though younger, healthy people without other medical conditions appear to be at low risk for serious complications.
How do you protect yourself? Are there ways to reduce the risk of getting COVID-19?
Unfortunately, as of this post, there is currently no universally accepted treatment for Coronavirus. The anti-malarial drug hydroxychloroquine, either alone or in combination with azithromycin (Z-pack) and zinc, was initially reported as a potential “game-changer” treatment, but the data on whether this truly helps are mixed at best, and hydroxychloroquine can have significant side-effects. Several studies have actually cast serious doubt on the effectiveness of hydroxychloroquine for COVID-19. A recent study showed the antiviral drug Remdesivir can speed up recovery from a severe infection. However, for now, the best approach by far remains prevention.
People who recently completed or are currently in treatment for breast cancer are at higher risk for complications if they become infected. These recommendations will help protect you and reduce your risk of becoming infected:
- Social distancing – stay away from crowds and try to keep a distance of at least 6 feet between yourself and others when in public. The easiest way of avoiding the infection is to avoid people who are, or could be infected. Remember, many people who get infected won’t develop symptoms for several days. Cancel any non-essential doctor visits. If you can, please just stay at home.
- Wash your hands with soap and warm water for at least 20 seconds multiple times a day, especially after any contact with others. Use an alcohol-based hand sanitizer (containing at least 60% alcohol) when soap and water aren’t available.
- Avoid shaking peoples’ hands.
- Avoid touching your face, especially your eyes, nose and mouth.
- Clean and disinfect surfaces you touch daily, including household surfaces, the inside of your car, doorknobs, light switches, and your cellphone; make sure you use cleaning products that are effective in killing viruses.
- Politely tell friends and family who are sick to stay away from you.
- Make plans with your family or support structure in case you get sick.
- Ask your employer to work from home if at all possible.
- Fill your prescriptions and think ahead to make sure you’re not caught short with medications you need daily.
- Catch up on groceries and Make sure you have over-the counter medications like Tylenol in the house.
- Disinfect your groceries before putting them away, and wipe down or spray your mail and packages with disinfectant before bringing them into the house.
- Avoid unnecessary travel on public transport or airplanes.
- Avoid contact with people who have recently traveled to a highly impacted area.
- Postpone all non-essential doctors’ visits like routine follow ups.
- If you absolutely must leave the house, wear a cloth face mask over your nose and mouth, especially when going to stores or other areas where social distancing (6 ft) is difficult to maintain, or you will be in an enclosed area like a grocery store. You do not need to use a surgical face mask, so please do not hoard them. Our healthcare heroes on the front lines are in dire need of masks and other personal protective equipment.
What should you do if you develop symptoms?
If develop a fever, cough, or shortness of breath, please call your doctor. Most people with mild symptoms will be able to stay at home while the illness runs its course. However, if you develop symptoms you should definitely let your doctor know, by phone first before going in to see them.
If you develop a fever, don’t use ibuprofen – there is evidence that it may make this infection worse. Stick with Tylenol but be sure not to take more than the recommended dose.
What if you have surgery scheduled soon?
The decision to proceed with surgery will ultimately depend on several factors that need to balance the details of your diagnosis, the urgency of your surgery, travel requirements, and the protocols your team and hospital have in place. ‘Elective’ (non-urgent and non-emergent) surgeries have been on hold for many weeks now. Some facilities are now starting to allow elective procedures again, but this varies tremendously based on the geographic situation. It is very important for you to discuss this with your medical team. Learn more about the impact of COVID-19 on breast cancer treatment here.
This too shall ultimately pass!
Ultimately, we must keep reminding ourselves that this too shall pass. However, the above risk-reducing measures will not only protect you, but will also help decrease the spread of the virus. Social distancing is the best thing we can all do right now while we wait for a proven vaccine, and staying at home protects you and helps limit the spread of the virus as much as possible.
This is a constantly changing situation, so please be sure to check the CDC’s ongoing updates regularly.
Weight-loss Surgery May Decrease Breast Cancer Risk
According to US Centers for Disease Control and Prevention (CDD), obesity is associated with an increased risk for 13 types of cancer, including breast cancer.
For individuals at high risk for developing breast cancer, maintaining a healthy lifestyle and BMI is important for reducing the likelihood of developing the disease. In some situations, weight loss surgery may be a good option to help reduce the overall risk.
According to a new study presented by Cleveland Clinic Florida researchers at the 36th American Society for Metabolic and Bariatric Surgery (ASMBS) Annual Meeting at ObesityWeek 2019, weight loss surgery cut the overall risk of developing cancers linked to obesity by 20%. In fact, women with obesity and known genetic susceptibilities for breast cancer were 2.5 times more likely to develop breast cancer than women with the same genetic risk who underwent weight loss surgery.
“Our findings suggest bariatric surgery could significantly prevent the development of cancer in patients with a higher risk than the average population, even in those genetically predisposed,” said study co-author Emanuele Lo Menzo, MD, Ph.D., FASMBS, Associate Program Director, General Surgery Residency Program, Cleveland Clinic Florida in Weston. “The effect we saw on patients genetically predisposed to developing breast cancer was remarkable and we believe this is the first time a study has shown such an impact. Further studies are needed to determine the factors, including weight loss, that may have led to such risk reduction.”
It is interesting to note that a similar study of patients with severe obesity (BMI of 35 or higher) published in Annals of Surgery earlier this year showed weight-loss surgery was associated with a 33% decrease in the risk of developing any type of cancer, and a 40% decrease in the risk of being diagnosed with a cancer associated with obesity.
It is important to remember, even individuals with a healthy BMI are still at risk for developing cancer. The importance of achieving and maintaining a healthy weight is to reduce the likelihood of developing breast cancer – unfortunately, it is NOT guaranteed prevention.
If you struggle to maintain a healthy weight, you are not alone! In fact, maintaining a healthy weight is a challenge for most adults today. The CDC reports more than 70% of American adults are overweight.
Maintaining a healthy weight is also very important after breast cancer treatment to decrease the risk of a recurrence. However, add the impact of a breast cancer diagnosis and the side-effects of some treatments, losing weight after breast cancer is typically even harder. Weight loss surgery may therefore also be an option for some survivors to consider if all other options have been exhausted.
Most people know that calorie control and regular exercise are crucial in losing and maintaining weight, but few people realize 80% of weight loss is achieved through better food choices. Even when we think we’re doing well by choosing the salad, we don’t realize the dressing has more calories than a Big Mac! A consultation with a nutritionist or dietician is a very good place to start your weight loss journey, and can provide extremely useful guidance in planning healthier meals.
Free App for Breast Cancer Treatment and Breast Reconstruction Decision-Making
A leader in breast cancer treatment education and shared decision-making, Breast Advocate® is excited to announce the release of our updated free app for breast cancer surgery and breast reconstruction. Thank you to our users for providing the valuable feedback that has helped make our app even better!

The latest updates greatly improve user experience and navigation, and give the innovative breast cancer app a fresh new look. Users can now customize the content they see on their dashboard via a personal feed, and easily find specific content using our optimized search engine.
Co-created by breast cancer specialists and patient advocates, the Breast Advocate® app provides anyone with breast cancer, a history of breast cancer, or at high risk for developing the disease a much needed voice in their treatment decision-making.
Should you have a lumpectomy or mastectomy? Should you have prophylactic surgery? Should you go flat or have breast reconstruction? If you want reconstruction, what type is best for you? Should you have gene testing? Our breast cancer app can help with these questions and much more.
The groundbreaking Breast Advocate® Wizard walks users through a detailed questionnaire to better understand their personal situation, preferences and goals. Our proprietary software combines evidence-based treatment options with the user’s preferences to create customized recommendations that are in line with the user’s specific needs. Breast Advocate® empowers users with the knowledge they need to fully discuss their treatment plan with their medical team and ensure they make the best decisions for them.
Users also have access to the latest expert opinions, published studies, helpful resources, and a community ready to provide support.
Download the latest version of the Breast Advocate app here.
Are Breast Cancer Risk-Reducing Medications Right For You?
With the exception of skin cancer, breast cancer is the most common cancer among American women, and the second leading cause of cancer deaths in the US. Women with a high risk of developing breast cancer have the option of lowering their risk by taking certain medications.
The US Preventive Services Task Force (USPSTF) recently made two updates to their recommendations for risk-reduction medications:
“The USPSTF recommends that clinicians offer to prescribe risk-reducing medications, such as tamoxifen, raloxifene, or aromatase inhibitors, to women who are at increased risk for breast cancer and at low risk for adverse medication effects”. This recommendation is for women who have never been diagnosed with breast cancer, but have at least a 3% risk of developing the disease within 5 years.
“The USPSTF recommends against the routine use of risk-reducing medications, such as tamoxifen, raloxifene, or aromatase inhibitors, in women who are not at increased risk for breast cancer… This recommendation applies to asymptomatic women 35 years and older, including women with previous benign breast lesions on biopsy such as atypical ductal hyperplasia or lobular hyperplasia, and LCIS. This recommendation does not apply to women who have a current or previous diagnosis of breast cancer or ductal carcinoma in situ.” In this group of patients, the side effects associated with taking these medications would likely outweigh the prevention benefit.
The USPSTF based its recommendations on the evidence of the benefits and potential side effects of taking any of these risk-reducing medications, and an assessment of the balance. The USPSTF does not consider the cost of care in any of their assessments.
The USPSTF also states that it recognizes that clinical decisions involve more considerations than evidence alone. We strongly encourage a shared decision-making approach between patients and their healthcare team to determine what’s best for you. If you would like to learn if you could benefit from taking a risk-reducing medication and whether taking one is right for you, please discuss the full range of options, risks and benefits with your physician.
You can read the full USPSTF statement here.
New Blood Test could predict Breast Cancer Recurrence and even prevent Surgery
While there is still much work to be done, detection and treatment of early stage breast cancer have improved tremendously over the last few years. Chemotherapy regimens have become increasingly effective, boosted by the emergence of immunotherapy, and often lead to a ‘pathological complete response’ when given before surgery (known as ‘neoadjuvant therapy’). A pathologic complete response means there is no identifiable tumor in the tissue that is resected by the lumpectomy or mastectomy.
However, there is currently no way to truly know which patients treated for early stage breast cancer enter remission and which ones actually have residual cancer cells in their system (in the absence of obvious metastatic disease).
A recent study published in Science Translational Medicine reported very encouraging news on a test called Targeted Digital Sequencing (or ‘TARDIS’) that could potentially help predict which patients are at high risk of breast cancer recurrence. TARDIS identifies DNA released by breast cancer cells into the bloodstream but is up to 100 times more sensitive than other liquid-biopsy tests currently available or in development.
This could be a huge step forward since TARDIS will potentially help doctors identify patients with early stage breast cancer who may still have residual cancer cells in their bodies after treatment that aren’t otherwise detectable by standard scans and follow-up monitoring.
It is also possible that the test could help remove the need for surgery altogether in women who experience a pathological complete response with neoadjuvant chemotherapy and are shown to have no residual breast cancer DNA in their bodies.
Very exciting news indeed! Read the full article here.
Will this detect breast cancer 5 yrs earlier?
MIT’s Computer Science and Artificial Intelligence Lab has developed a new tool that uses artificial intelligence (AI) and deep learning to predict the development of breast cancer up to five years earlier than current detection techniques.
Unlike other AI-based tools that use data mostly from acquired from white patients and may therefore be algorithmically biased, MIT’s model works equally well for both white and black patient populations. This is particularly important as black women are 42% more likely to die from breast cancer than white women – a possible contributing factor could be that current detection techniques don’t work as well in black women.

To create the tool, data was obtained from over 90,000 mammograms and outcomes from over 60,000 patients treated at the Massachusetts General Hospital. A form of machine learning known as “deep learning” was then used to identify patterns in the images and data that are too subtle to be routinely recognized by human physicians. The results have so far have been more accurate than current diagnostic approaches, presumably because the model is not based on existing knowledge and assumptions about patient risk factors.
MIT’s project is intended to help doctors compile the best personalized screening program for their patients and hopefully eliminate the heartbreaking outcome of a late breast cancer diagnosis. We eagerly await to hear if and when this could become widely available.
New surgical guideline leads to lower re-operation rates after lumpectomy surgery
Re-operation rates following breast conservation (lumpectomy and radiation) for early invasive breast cancer have been highly variable historically, mainly because of uncertainty and variability in what surgeons deemed safe.
When a tumor is removed, the specimen is painted with a special ink before it is evaluated by a pathologist. This ink allows the pathologist to clearly see the outer edges, or ‘margins’, of the tissue under the microscope.

In 2014, the Society of Surgical Oncology and American Society for Radiation Oncology released new guidelines stating that as long as the tumor has no ink on it, the margin is clear. A clear margin means there are no cancer cells at the edge of the surgical specimen and tells the surgeon that all the cancer was removed.
Prior to the new guidelines, some surgeons wanted at least 2mm of normal breast tissue around the cancer. Others accepted less. Even though wider clear margins don’t reduce the risk of cancer recurrence, because of this lack of consensus, 25%-30% of patients having a lumpectomy required more surgery to ensure a larger clear margin.
A recent study in the American Journal of Surgery shows that the new guidelines have led to a decrease in re-operation rates. This offers peace of mind that you likely won’t need another “re-excision” surgery after a lumpectomy if the margins are clear, irrespective of how small the clear margins are, as long as there is “no ink”. Additionally, surgeons now have an evidence-based standard to follow. Very reassuring news indeed!
Does DIEP flap breast reconstruction increase the risk of breast cancer recurrence?
Patients choosing to undergo breast reconstruction are often concerned that their decision may increase their risk of breast cancer recurrence. A recent study published in the British Journal of Surgery looked at the risk of recurrence specifically after DIEP flap reconstruction.
The study compared 250 patients who had DIEP flap reconstruction between 1999 and 2013 with more than 700 control patients. Breast cancer recurrence was seen in over 19 percent of patients who had DIEP flap surgery and over 23 percent of patients in the control group. Interestingly, the 5-year breast cancer-specific survival rate was highest in patients having DIEP flap surgery after 2008 – 92.4 percent in the DIEP flap group versus 87.4 percent in the control group.
The study design does raise some questions about selection bias. For example, all DIEP flap procedures in this study were performed at least 24 months after mastectomy. No DIEP flaps were performed at the same time as the mastectomy (‘immediate’ reconstruction). In addition, a larger number of patients in the DIEP flap group than the control group received adjuvant therapy.
While the survival rates between groups may have been influenced by patient selection, this study shows that patients with breast cancer undergoing DIEP flap breast reconstruction do NOT have a higher rate of breast cancer recurrence than patients undergoing mastectomy alone.
Robotic Mastectomy – a natural evolution or a huge safety concern?
Robotic nipple-sparing mastectomy was first described in 2015 and appears to be gaining traction in Europe. Slower to catch on in the US, the procedure is now also starting to raise safety concerns for some surgeons.
The da Vinci robot is not yet FDA-approved for mastectomy. There is concern amongst some medical professionals that robotic tumor removal could inadvertently cause breast cancer cells to spread by fragmenting the cancerous tissue as it is being pulled out of the small incision.

Dr Hooman Noorchashm, a Philadelphia-based surgeon turned patient advocate, has raised questions about the safety and appropriateness of using the da Vinci robot for mastectomies… “The reason why I am focused on robotic mastectomy is because I think there is a parallel [with hysterectomy via power morcellator] of selling cosmesis and convenience to women for a surgical operation. The US Food and Drug Administration (FDA) has a history of being lax in its oversight of 510K devices, which include the power morcellator and the da Vinci robot, he said. These devices can replace established standards of care without proper evidence.”
To date there have been no clinical trials to compare the safety of robotic surgery with the traditional techniques used for breast cancer surgery.
Dr Noorchashm has also referred to a recent study from MD Anderson that compared survival rates of laparoscopic hysterectomies for cervical cancer to traditional “open” surgical methods that use larger incisions. The research found that patients who underwent the minimally invasive laparoscopic surgery were four times more likely to experience recurrence than those who had the open surgery. These finding came over 10 years after laparoscopic surgery was recommended as the standard for care.
This is not to say that robotic surgery isn’t an option for some patients. Recent headlines have praised surgeons for performing robot-assisted prophylactic breast surgery and immediate implant-based breast reconstruction. Although controversial, there is no evidence to suggest robotic surgery could increase the risk of developing breast cancer in preventative mastectomy cases.
Long-term, high quality research is underway, but it could be years before there is a better understanding of the full impact and risk of robotic surgery for breast cancer patients.
Looking for more information to help you weigh your surgical options? Download the Breast Advocate app now.
Addendum 2/28/19:
FDA issues safety communication about robotic mastectomies – Caution When Using Robotically-Assisted Surgical Devices in Women’s Health including Mastectomy and Other Cancer-Related Surgeries.




