COVID-19 Patient Outcomes After Breast Cancer Treatment
Scientists and medical professionals are continuing to learn more about the new Coronavirus strand that has changed our world today. For breast cancer patients, compromised immune systems following treatment place them in the “high risk” category for contracting COVID-19. Likewise, they may also have a higher risk of developing more sever symptoms. However, a recent study sheds a small positive light in the otherwise overwhelming reality of the current pandemic. The study analyzed COVID-19 mortality among patient who had undergone previous breast cancer treatment.
Seventy-six breast cancer patients were enrolled in the study, of which 59 had COVD-19. Of the positive coronavirus enrollees, 37 had metastatic breast cancer, 28 required hospitalization, 6 required admittance to the ICU and 4 died. Results showed COVID-19 deaths were more likely due to other comorbidities rather than current or previous breast cancer treatments. Of those patients who sadly lost their lives, all had significant noncancer comorbidities including hypertension, obesity, diabetes and heart disease.
“While our study cannot determine the incidence of COVID-19 infection among breast cancer patients, the small number of diagnosed cases suggests that breast cancer patients do not appear to be at higher risk than the general population,” the authors of the study share in the findings summary. “Importantly, we found no trend in favor of a relationship between a history of breast and lymph node radiation therapy, radiation therapy sequela, and radiologic extent of disease or outcome.”
Although breast cancer patients need to take every precaution possible to reduce the risk of contracting and spreading COVID-19, if a positive diagnosis does occur, prior breast cancer treatment will likely not impact recovery.
According to the CDC’s guidelines, it is very important we all take the following steps to reduce the risk of contracting and/or spreading COVID-19:
- Wash your hands often
- Avoid close contact with others
- Cover your mouth and nose with a mask or cloth covering when around others, especially indoors
- Cover all coughs and sneezes
- Clean and disinfect surfaces regularly
- Be alert for symptoms and take your temperature regularly
Breast Advocate Founder Answers Your COVID-19 Breast Cancer and Breast Reconstruction Questions
Breast Advocate founder Dr. Minas Chrysopoulo recently answered patient questions on all things COVID-19 and breast cancer/breast reconstruction live on Facebook. During the educational hour, ‘Dr. C’ touched on topics ranging from how Coronavirus is spread, who is at high risk and the impact this outbreak is having on breast cancer surgery and breast reconstruction scheduling. Catch the replay here…
Question: What is COVID-19?
Answer: COVID-19 is the disease caused by the Coronavirus. The formal medical name for the Coronavirus is “SARS CoV-2”. It’s important to note that this virus has nothing to do with the flu. It’s been compared to the flu, but it’s not actually a type of flu. It’s not an influenza virus (the virus family that causes the flu), but some of the initial symptoms can be similar. The symptoms of a COVID-19 infection can be fever, a dry cough, shortness of breath especially on exertion (if you’re doing something that’s usually easy and all of a sudden you’re a bit short of breath, then this may be the first symptom you have), fatigue, poor appetite, headache, and some people also have GI symptoms like diarrhea. Please don’t go and hoard toilet paper…there’s really no need! It’s important to bear in mind too that at least 25% of people who become infected with the coronavirus never develops symptoms. That’s why social distancing is really important! Stay six feet from anyone when you leave the house. Obviously inside the house with your loved ones it’s very difficult to stay six feet away and there’s really no need to social distance from them, unless there’s a concern a family member has been exposed. In that case, please try at all costs if it’s possible to separate that individual from the rest of the family.
A lot has been made of the fever because it’s such a common symptom. However, you don’t need to have a fever to have COVID-19. In fact, all of those symptoms I mentioned above can occur on their own. For example, I have a very close friend who was recently admitted to hospital for care and he just felt fatigued for many days before the shortness of breath started. He never actually had a fever at all and we are hearing about more and more of those cases.
Question: How is COVID-19 spread?
Answer: First and foremost, this is a respiratory disease. The virus attacks your lungs first before it attacks anything else. That’s how it really tries to get a hold of your body, through your lungs. Coughing, sneezing and even breathing can spread the virus. Anything that releases droplets into the air can spread the virus. That’s why social distancing is really being emphasized because the best way to protect yourself is to stay away from others — at least six feet. You can also develop the inflection through touching someone who’s infected or by coming into very close contact… The virus can get on your hand and then enters your body when you touch your face. If you touch your mouth, your nose or your eyes that’s how the virus gets into your system, because it was on your hand.
Coronavirus can stay alive outside the body for many hours, and depending on the surface, up to many days. Metal surfaces in particular can have corona virus on them (eg doorknobs and shopping carts). The virus can stay on metal up to 3-5 days according to some studies. When you look at the cruise ship data, there’s some evidence that the virus can live up to nine days. If that’s true it probably has to do with environmental conditions like sunlight and heat. We just don’t know quite frankly, but what we do know is the virus survives on metal for at least three days. So if you have to go to the grocery store wipe down the cart. I would also recommend that you wear gloves. There’s been a shift in terms of the recommendations for face masks. Initially the CDC and the World Health Organization stance was that you didn’t need to wear a face mask unless you were sick. The reason for that being that face masks really weren’t that protective if you weren’t sick already and the reason to wear a mask was basically to keep the virus to yourself and to prevent spreading it. But I’m sure those of you who have been watching the news and the images from around the world from the countries that have dealt with the virus more successfully than the US (places like South Korea, Hong Kong, Singapore), the public is walking around with masks. Now the sense is that there’s something to that and even though face masks won’t protect you 100%, the recommendation now has shifted. I would say if you’re going out to a store or grocery store wear a mask of some sort. If you don’t have a mask wear a bandanna over your nose and your mouth. It’s better than nothing. I do feel very strongly that we have to prioritize the safety of our first-line health care workers. A lot of them are dealing with patient after patient who are infected. Our first-line health care workers must be prioritized in terms of surgical face masks and other personal protective equipment. But, in terms of what our patients should do…if you have a cloth mask at home — use it.
Question: What can individuals do to protect themselves?
Answer: In addition to what we’ve just said, think about what you’re touching. Hopefully you’re all social distancing and are staying at home. If you’re not, you should be. It’s the only way to stop the transmission. If you think about people as dominoes, when you line up dominoes and then you flick the first one, each domino falls over one after another after you flip the first. Now imagine each domino is a person. The virus spreads from person to person, just by being close to each other. The first person who gets infected potentially infects three other people. The only way to stop the dominoes from falling is to move a couple of dominoes out of the way so that when a domino falls it doesn’t touch the next one and doesn’t push the next one over. That’s how social distancing works — the infection stays in those who are infected, doesn’t spread, and eventually it dies out and that individual hopefully gets better. Most people do get better! For 20% of people who get symptoms, the symptoms are mild. Another 20% of folks will have more severe symptoms but probably won’t need to be hospitalized. It’s only about 10-15% of people who get the infection that will need hospital care and of those, it’s about 5% that will have severe breathing problems that will potentially need the intensive care unit and ventilator support.
Question: Who is at risk for developing severe symptoms?
Answer: The elderly and people with underlying medical problems are most at risk. This includes those who have compromised immune systems. So obviously, patients with cancer are very much on that high-risk list. Now, if you’re a ten-year survivor or you’re ten years out from chemo, you’re not considered immunocompromised anymore and you’re not high risk. But, if you’ve just finished chemotherapy you’re high risk. If you’re going through cancer treatment right now, if you have a current cancer diagnosis — you’re high risk. If you’re over 60 yrs old, you’re high risk. If you have underlying medical problems like heart disease, lung disease, kidney disease, diabetes, asthma,.. you’re at high risk. So, you must protect yourself and really minimize your contact with the outside world. Minimize doctor visits as much as you can. Obviously, that’s impossible if you’re still undergoing cancer treatment and you need to go in to see your oncologist. But, if you’ve finished treatment or you’re not getting active treatment right now, don’t go for a routine screening mammogram or ultrasound. All those things can wait. The American Society of Breast Surgeons has recommended very strongly that all screening tests to be postponed.
Question: Why have hospitals cancelled breast reconstruction surgeries?
Answer: There are a bunch of recommendations now from American societies, including the American College of Surgeons, the American Society of Breast Surgeons and the American Society of Plastic Surgeons. Any breast cancer care that doesn’t involve surgery is essentially being prioritized wherever it’s safe to do so. If there’s any possible way you as a breast cancer patient can be treated right now without surgery initially, without it impacting your prognosis, then that’s the recommendation. For example, if your cancer can be controlled by hormone therapy, an aromatase inhibitor or you can have neoadjuvant chemotherapy first before your surgery, all that’s going to be prioritized. We want to keep people out of hospital as much as possible. The last thing breast cancer patients who are immunocompromised need is to go into surgery and be exposed to the virus. As I said, this affects your breathing, your lungs,.. your respiratory system. The last thing you want to do is go in for a surgery that could have potentially been delayed a little bit and then you end up on a ventilator because you contracted the virus. This is also about preserving resources to get all the COVID-19 infected patients through this and minimize the death rate. But please know, this decision from our societies in terms of breast cancer care is to protect you. Please remember that as a result, breast reconstruction (because the surgery is not immediately life-saving) is going to be postponed. Certainly here in Texas that’s the position. Ultimately your situation will depend on your diagnosis, stage and where you live (depending on the geographic situation and how bad things have gotten). It may also depend on your state laws. There have been several state laws that have been passed that prevent certain surgeries. Please talk to your medical team your and your surgical team about your specific situation. But generally-speaking, breast reconstruction is on hold because it’s not immediately life-saving. Unfortunately that really does prolong the process for many people. Lots of patients have now been caught in limbo but you will get through this. You will get your surgery. I don’t know when things are going to be back in terms of scheduling. Certainly for us, we’re looking at this in two week increments moving forward and it’s a very fluid situation. The infection numbers are changing, the projections are changing. It’s a day-by-day thing. We just have to prioritize everyone’s safety.
Question: When will people being rescheduled for surgery?
Answer: All I can say right now is people will be rescheduled as soon as it’s safe to do so.
Question: Can you get the virus again if you’ve already been diagnosed?
Answer: We think that if you get it once that you’ll be okay for this season. I mentioned at the beginning that coronavirus has been compared to the flu. In terms of immunity, it probably is quite similar. When you get the flu it doesn’t mean you can never get the flu again, but it does mean that if you do get the flu again it won’t be quite as severe. Your immune system does protect you somewhat for the following season. Obviously the flu shot is a big help! I’m not going to get into the whole pros and cons of vaccination. Personally everyone in my family will always be vaccinated because vaccines work. But let’s not talk about the pros and cons of vaccines here. Hopefully the vaccine for coronavirus or for COVID-19 will be available soon. When you look at how long it takes to develop a vaccine (and several companies are working on it already), realistically it’s not going to appear I don’t think before the beginning of next year at the very earliest. It looks like if you get COVID-19 now you should be okay and you probably not at risk of getting it again for a while. But we don’t know for sure how long can someone be a carrier. I don’t know the answer to that because without widespread testing we don’t know who is a carrier so we don’t know how long they’ve been carrying it. If you look at the lifespan of the disease, if you get through two weeks (which is why for folks who are in quarantine it’s two weeks to make sure that it that they don’t develop any symptoms) we think the virus kind of burns itself out. There have been a small percentage of people who have become infected and ultimately didn’t develop symptoms until beyond two weeks but that’s only about 1% of people who have been infected as far as we know.
Question: Is there any medicine that we can take to help?
Answer: No treatments have been proven to be reliably effective so far. Obviously there’s a lot of hope being put on hydroxychloroquine, a z-pack, and zinc as a cocktail but the data on that is very poor to be honest. In terms of vigorous scientific data, if you develop symptoms the only thing you can do really it’s make sure you stay well hydrated, and make sure you’re still eating as much as you can, and stay mobile. Don’t stay in bed. It’s supportive measures only really.
Question: Is there a blood test for antibodies to determine if you’ve already had COVID-19?
Answer: Yes. It’s coming. It’s not going to be widely available for a while, but yes.
Question: If someone completed radiation treatments eight years ago and they are 65 and they have a compromised immune system should they be going to work?
Answer: I wrote an article that’s published on BreastAdvocateApp.com. It’s about what coronavirus is and what breast cancer patients should know. There’s a whole list of precautions and advice, and one of those is if there’s any way you can work from home, do it. Again going back to social distancing…you know we’re at the point where this isn’t going to go away on its own. There cannot be life as usual. The best thing anyone can do to protect themselves is limit their risk of exposure. The only way to do that is to stay home and leave the house only when you absolutely must. When you go out be a minimum of six feet away from everyone. That means most people should be staying at home and working from home if that’s at all possible. Now I fully appreciate that unless it’s mandated by your individual state it’s very much left up to your employer, but please push it as much as you can to work from home.
Question: I was supposed to have prophylactic surgery this year but it’s been postponed. Should I ask my doctor about going on tamoxifen?
Answer: That’s a great question. Anyone who has a high-risk gene mutation, anyone who carries a gene mutation like the BRCA mutation (which is obviously the best known but certainly not the only one), should talk to their physician about steps that they can take that don’t involve surgery to see them through, until the point where they can get the risk-reducing surgery they want. Please also remember that non-surgical methods of risk reduction are chosen by a lot of people right off the bat. It’s a very valid way to go to decrease your risk. As I mentioned earlier, the screening aspect of it is going take a hit for the next few months, but you can definitely go on risk reducing medications like tamoxifen if you choose. That’s another option.
Question: If it does not impact prognosis and local hospital resources allow for a choice between hormone therapy or a mastectomy is it still preferable to opt for immediate mastectomy with DIEP flap later?
Answer: Well if it doesn’t impact your prognosis then you can also look at it the other way and ask, ‘why have the mastectomy if that can be delayed.’ From a strictly cosmetic standpoint, immediate reconstruction is going to be better. In some places you can still have your mastectomy and have a tissue expander placed. The tissue expander preserves the skin envelope and you can later have that expander exchanged for your DIEP flap, so in that sense you do get an extra surgery because the DIEP flap and the mastectomy aren’t being performed at the same time, but the tissue expander is used as a bridge between the two. Whether that’s an ‘acceptable’ way to go or not will depend on where you are and the situation.
Question: Once we get back to normal and you are allowed again to do surgery, how long would it take to be scheduled again?
Answer: Great question! But I don’t really know. I promise and surgeons across the globe will get everyone in as soon as they can. Unfortunately, some of you will have to wait a little bit longer then you want to wait, but we’re going to get everyone through as soon as physically possible. I promise!
Question: What is your advice for staying healthy while patients are waiting for the DIEP flap procedure and sheltering in place?
Answer: Great question! Nutrition and exercise! Don’t start any bad habits. Don’t start smoking. You can still drink, just use your best judgment and also obviously follow your medical oncologist’s guidelines in terms of alcohol because you may be on some other medications…it depends on what part of your treatment you’re in, etc. Just try to eat as healthy as possible and exercise. Aerobic exercise always improves healing so try and get some exercise in if you’re waiting for a DIEP flap. Specifically remember what your surgeons told you in terms of where you are with your specific weight. Sometimes losing a significant amount of weight can hurt you in terms of the DIEP flap procedure and how much tissue can be moved, and how much tissue there is to work with,.. or any other flap procedure for that matter. So I wouldn’t necessarily prioritize weight loss but I would prioritize healthy living as much as possible.
Question: What should individuals do about abdominal wounds that aren’t healing properly during this time?
Answer: It depends on the practice that you’re in, who your physician is and how they do it, but I’ll tell you how we’re doing it in my practice, PRMA. If one of my patients has a wound healing problem, the first thing we’re going to do is get on a telehealth visit and take a look at things to see how things look. Not all healing problems are the same, so if we see that it’s just a little bit of superficial scabbing or something like that, then a little TLC is all the patient needs. That person isn’t going to have to come in and increase their risk of coronavirus exposure by coming into a medical office. If it’s something that looks like it needs to be cleaned up and we need to maybe cut away a little bit of devitalized tissue to help things heal, then we’ll have you come in. We’re evaluating on a patient by patient basis. Let me also backtrack a little bit and tell you what we’re doing in the office again in case you do still have to come in for an in-person visit. Let’s say you do have a wound healing problem or we’re worried about an infection, or anything that cannot be dealt with over telehealth. We, for many weeks now, have been following the most aggressive approaches in terms of minimizing patient risk in the office so please be prepared. The nurse and the physician wear masks and gloves. It’s not personal, it’s for everyone’s protection. Everything is cleaned with antiviral detergents between every patient visit. Patient visits are staggered so the only person (other than your medical team) who will be in the office when you’re there will be you, unless it’s impossible to avoid that situation. That’s always going to be the primary goal. If there’s someone else already in the office and you have to wait a little bit for the appointment then you’ll be asked to wait in your car, and we will text you or call you (whatever works best for you) when we are ready for you to come in. We’ve got this really streamlined now. We take this exceptionally seriously and we’re only going to be bringing you into the office if we absolutely have to.
Question: I am a five-year survivor with asthma and on tamoxifen. Am I considered high-risk?
Answer: Yes, anyone with a breathing issue like asthma, chronic bronchitis, COPD, smokers, anyone who vapes, are higher-risk. You don’t have to smoke cigarettes; it includes pot as well. Anything you inhale other than air increases your risk because it really decreases your capacity to deal with a pulmonary insult. Anything that attacks your lungs is going to have an easier time if your lungs are compromised because you inhale stuff you shouldn’t on a regular basis. We have seen a lot of younger folks be hospitalized and we think that some of that is the extent of vaping in that age group.
Question: I am two-weeks post-op double mastectomy with DIEP flap. Because of COVID-19, will my phase 2 surgery be delayed?
Answer: Yes, all surgeries are off right now. So yes, unfortunately your revision surgery will be delayed. For surgery in our practice, most breast reconstruction patients get a second stage, or ‘tune-up’ surgery. Step one, the first surgery, is about making patients physically whole again. The second surgery is about making them look as good as possible. This addresses symmetry issues, size discrepancy, contour issues after mastectomy, and maybe some unevenness and scarring. If you have had DIEP flap surgery, we address the belly scar to smooth things out and smooth out the belly contour; basically, make things look as good as possible, that is stage two. So yes, all stage two surgeries are also delayed.
Question: Since I was scheduled for this week, I have been following pre-op instructions, should I continue?
Answer: That’s a good question, some of them you’ll need to continue, others not so much. Please email your surgical team and go through the list to see which of those you really need to be continuing, and which of these you can put on hold for now.
Question: I am assuming that the length of time for a tissue expander placement is not a problem? I have some family members that are concerned I have had a tissue expander in place for 2 years, and now it is up in the air – is there a limit on how long the tissue expander can be in place?
Answer: No, if you’ve got a tissue expander in place and you are not having any issues, you can keep that in for as long as you need to. So no, it is not a medical concern. It doesn’t impact your health if you’ve got no problems with it whatsoever. Rest assured, there is no urgency from a medical standpoint or health perspective. I know you’re probably dying to get it out, but medically speaking you’re fine.
Question: Can you demonstrate proper hand washing?
Answer: I can try. Okay, take off your jewelry. Warm water and soap will do it. Quite frankly if you’re in the kitchen and you’ve got dish detergent, that will work too. Warm water, and you’ve got to wash your hands for at least 20 seconds. There have been some pretty amusing songs on social media of people picking different songs. Do whatever you need to do that lasts 20 seconds to guide you. You get your hands wet with warm water, add the soap or detergent, lather up, get a nice foam. I would treat this kind of like a pseudo-surgery scrub. You know when we prepare for surgery, we obviously do a lot more than this, but this is kind of a pseudo-surgical scrub. So once you’ve done that for a few seconds, focus on every finger, and both thumbs, all the way around each finger, all the way around both thumbs. Then you rub one hand on top of the other, because you need to do that to really get into the web-spaces. Every web-space, and then again on the other side once again to finish off. Then get your jewelry, rinse that and wash it really well. This ring is metal, and the virus can live on metal for several days as we discussed earlier. So wash It really well, then put it back on and dry your hands. That’s it! 20 seconds, warm water, with soap!
Question: What is the optimal BMI for DIEP flap surgery?
Answer: Good Question. The optimal is high 20’s from a surgeon standpoint. When you get up to 25, this is the normal BMI, as DIEP flap surgeons, we like when patients are a little bit heavier, it’s a little bit easier to get more volume obviously. However, I wouldn’t encourage gaining weight. I really avoid doing that at all costs just to make someone a candidate for surgery. Some people are happier at a slightly higher weight and that is just fine. It gets harder to do DIEP flaps when the BMI starts to get down towards 20. Most women can still get a DIEP flap with a BMI of 20, but a lot of it obviously depends on how you carry the tissue that you do have, and where it is on your body. Some ladies with a BMI of 21 that have had a couple of kids, and they’ve got a little pooch as they call it. I had a lady the other day that referred to it as a kangaroo pouch, which I hadn’t heard before but that works too. Anyway, some tissue that they wouldn’t mind getting rid of, if that is over the lower abdomen we can use it. Now ultimately, in addition to how you carry your tissue, another big factor is your breast size and what your expectations of final breast size are. Also, whether you will reconstruct one breast or two. So a lady who is very thin, who needs one breast reconstructed who wants to keep the other to preserve sensation, or because the risk of the other breast is low,… in that situation we can use all the lower tummy for just the one breast. That’s often referred to as a ‘stacked flap’. But even ladies having bilateral procedures, so both breasts, can often have DIEP flap surgery even though a lot of surgeons will say “oh, you’re too thin”, or “you’re not a candidate”. It really does depend on how you carry your tissue. Even lower BMI patients, in the low 20’s can still be DIEP flap candidates. We see a lot of people in our practice who have been told elsewhere that they’re not a candidate for DIEP flap surgery for a variety of reasons. Previous abdominal surgeries,… very few prevent DIEP flaps from being possible. Certain types of abdominal surgery, if you have had a previous full tummy tuck, you’re not going to be a DIEP flap candidate, or if you’ve had major abdominal reconstruction you probably won’t be a DIEP flap candidate. There are a couple of those instances that we’ve pulled off too, but it depends very much case-by-case. If you really feel that DIEP flap surgery is for your, and you definitely want to look into it, if you’ve been told you aren’t a good candidate; I strongly recommend a second opinion. A second opinion can never hurt, even if it’s just to confirm what your first opinion was, at least then you know. Please by all means hit us up for a second opinion. We are here for you. We see a lot of people and talk to a lot of people who want a second opinion. Please use the PRMA Virtual Consultation form if that’s something you feel would be helpful for you. The other thing about DIEP flap and BMI is we tend to push the envelope in terms of high BMI and that is based on work that came out of our practice. That is a study we did that was led by Dr. Ochoa. So we looked at complication rates, and we found that patients with a BMI of up to 40 are candidates for the procedure. Above a BMI of 40 the complication rates really uptick. So the higher the BMI, the higher the line goes (in an upward motion). The higher the BMI, the higher the risk of complications. When the BMI gets to 40, the line stops being a gradual increase and heads more vertically. Now again, it depends on how you carry your weight. There are some ladies who have a BMI of less than 40 but the way they carry their weight; their risk will be more like a lady who has a BMI of over 40, so it is very much a case-by-case decision. This is the guide, so we really try to get our patients below 40 for DIEP flap surgery, it is just safer for the patient.
Question: What different platforms are you using for telemedicine and is insurance covering telemedicine?
Answer: There are several platforms — Skype and FaceTime are the two most popular. We are able to do it in a way that we don’t document anything in either of those platforms. Everything is documented straight into our EMR (electronic medical records) from a HIPPA protection standpoint. Skype and FaceTime are the most common platforms that we are using. Most insurance plans are covering it, but please confirm with your specific insurance carrier, so Please do check with your individual insurance carriers and plans to make sure that is the case.
The Impact of COVID-19 on Breast Cancer Treatment
Published March 31, 2020. Updated April 10, 2020
Breast cancer does not take a break…even amid a global crisis like the Coronavirus pandemic. For most people, it’s already overwhelming to hear the words “you have breast cancer”. In the midst of the current COVID-19 outbreak, increased uncertainty and changes in treatment recommendations are elevating everyone’s anxiety further. Many people are now being told that their treatment plan is changing. If you’re one of them, please know that your breast cancer team is adjusting your treatment plan to keep you safe and limit your exposure to coronavirus. Breast cancer patients are at increased risk of severe symptoms if they get coronavirus. People with severe symptoms need admission to a hospital for supportive care and are more likely to need intensive care, ventilator support for severe breathing problems, and are also at increased risk of death.

A recent study published in the Lancet, a highly respected medical journal, evaluated 34 patients who were infected with Coronavirus but didn’t have any symptoms, and underwent elective surgery. All developed pneumonia and 20% died.
All the medical and surgical societies are prioritizing your safety during this pandemic. At the same time as maximizing your safety, your team won’t do anything that negatively impacts your long-term prognosis.
Individuals Needing Chemo and/or Radiation
Most facilities providing chemo and radiation therapy treatment for breast cancer patients remain open and necessary treatment is not being delayed. Vigilant cleaning, health screenings of all patients before they enter the facility, and the advisement of patients to wear masks are just a few of the many steps healthcare workers are implementing to ensure patient safety. In many places, patients are no longer allowed to bring someone with them during their chemo treatments.
Individuals Requiring Breast Cancer Surgery
COVID-19 is impacting the surgical plans of many patients. At this time, the White House and numerous surgical societies are issuing guidelines recommending all surgeries that are not immediately life-saving be postponed. The American College of Surgeons and the American Society of Breast Surgeons are recommending delaying any surgery where a 6-8 week delay would not impact clinical outcomes. This includes surgery for DCIS, stage one ER/PR+ invasive cancers, re-excisions, surgery for high-risk lesions, and prophylactic (risk-reducing) mastectomies. Wherever possible, patients are being treated with hormonal therapy (eg Tamoxifen), aromatase inhibitors, or neo-adjuvant chemotherapy to enable surgery to be delayed. Recommendations are also calling for scheduled mastectomies to be converted to lumpectomies when clinically acceptable. Patients still wanting a mastectomy (with or without reconstruction) will be able to return for their definitive surgery once the crisis has passed.
Individuals Choosing Breast Reconstruction
For patients wanting breast reconstruction, there will unfortunately be a delay between the lumpectomy/mastectomy and the reconstruction procedure in most situations. In the US, some institutions are still allowing tissue-expander reconstruction, but the American Society of Plastic Surgeons (ASPS) strongly advises all autologous (flap) reconstructions be delayed. Although breast reconstruction is considered medically necessary, it is not immediately life-saving. For many, delaying reconstruction is understandably devastating, but it is important to remember there is no deadline for reconstruction and your health and safety are the top priorities of your surgical team.
Although reconstructive surgeries around the globe are being postponed, patients can still use this waiting period to research all their reconstructive options to determine which procedure is best for them. The Breast Advocate app provides personalized evidence-based information and recommendations for breast cancer surgery and reconstruction, after taking your situation and personal preferences into account.
Individuals at High Risk
At this time, individuals interested in prophylactic (risk-reducing) surgery because they are at high risk for developing breast cancer (eg BRCA+), should continue to self-monitor for breast changes at home. All society guidelines are strongly urging all prophylactic surgeries be postponed. Screening mammograms and MRIs may be delayed in your location during this pandemic. If any concerning breast changes occur, call you healthcare provider for further diagnostic instructions. Please also talk to your physician about the option of taking tamoxifen to decrease your risk while you wait for surgery.
It is important to remember that we must all do our part to protect ourselves, our loved ones, and our healthcare providers during this overwhelming time. By taking these measures, your risk of contracting COVID-19 will be minimized, hospital admissions will be reduced, necessary PPE will be conserved for our healthcare providers on the front lines, and lives will be saved.
Coronavirus: What Breast Cancer Patients Need To Know
Originally published March 12, 2020. Updated May 2, 2020.
With the spread of Coronavirus increasing across the US and other countries, it is essential for breast cancer patients and individuals with underlying health conditions (eg heart, lung or kidney disease, diabetes, asthma) that compromise their immune system to be educated and proactive in taking steps to protect themselves from contracting this new disease. Breast cancer treatments like chemotherapy, targeted therapies, immunotherapy, and radiation make the immune system weaker. People who have weakened immune systems have a much higher risk of complications if they become infected with this virus. In addition to the common sense precautions we should all take to prevent infection, people who have recently completed or are still undergoing cancer treatment should be extra vigilant as they are at a higher risk of hospitalization, severe complications, and even death.
What is Coronavirus?

The coronaviruses are a family of viruses that cause illnesses ranging from the common cold to more serious respiratory diseases. Flu is caused by a different virus (influenza). There is no vaccine for this coronavirus yet and it will be several months before a vaccine is available.
The disease caused by Coronavirus, known as COVID-19, is a respiratory illness caused by a coronavirus previously only found in animals that was first identified in an outbreak in Wuhan, China, in December 2019. The disease is spread through mucus droplets from the nose or mouth that are released when an individual close to you coughs or sneezes. It is also possible that a carrier of the virus can infect others by simply exhaling close to them. The infection can also be spread by touching a surface that mucus droplets have landed on, and then touching your eyes, nose or mouth. Coronavirus can stay alive on surfaces outside the body for many days, depending on the surface (72 hrs – 5 days). The virus likes metal surfaces like door knobs, silverware and jewelry in particular (survives for 5 days).
It appears the Coronavirus is much more contagious than the Flu. People seem to be most contagious when they have symptoms, but you can also catch the virus from infected people who have no symptoms. At least 25% of people infected with Coronavirus won’t develop any symptoms at all, and can very easily unknowingly spread the virus. Those who do develop symptoms take on average 5 days to do so. For these reasons, Coronavirus is spreading much faster than the seasonal flu.
What are the symptoms of COVID-19?
Most people who become infected with coronavirus have mild respiratory symptoms, and some people will show no symptoms at all. However, symptoms can become severe in some people, and some have died from the illness.
Similar to symptoms associate with the flu or common cold, the most common symptoms of COVID-19 include fever, a dry cough and shortness of breath. The CDC recently added the following list of possible symptoms: chills, repeated shaking with chills, muscle pain, headache, sore throat, and new loss of taste or smell. Any of these symptoms can range from mild to severe.
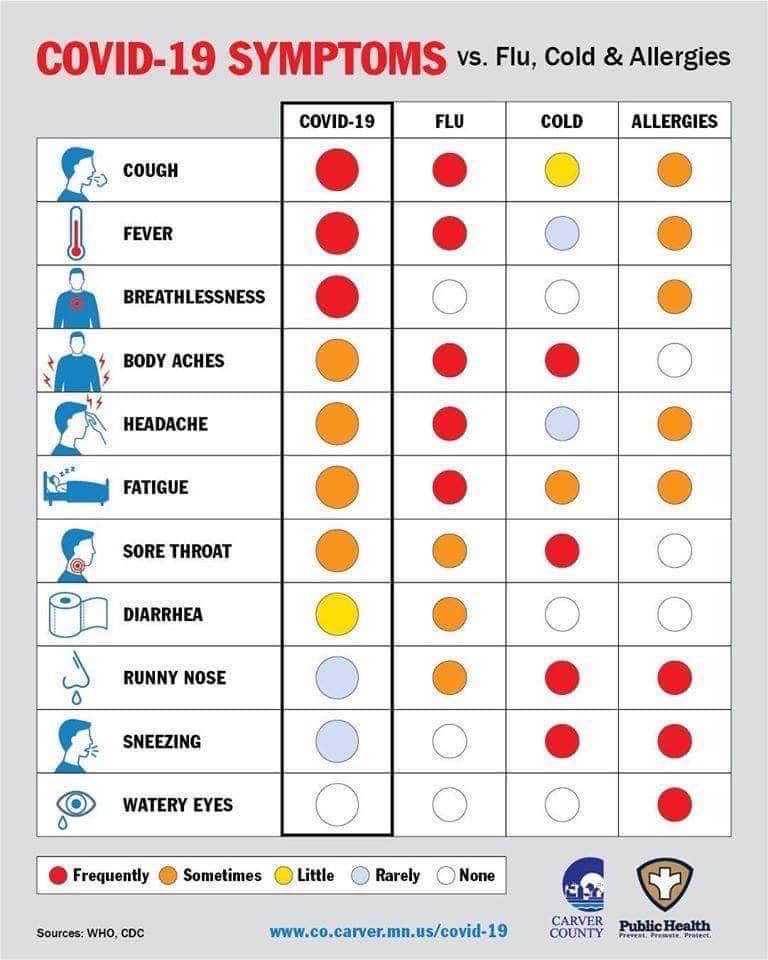
It is the impact on the lungs that doctors are most concerned about. According to the WHO, in people who have symptoms, about 40% will have mild symptoms, while 40% will develop mild to moderate pneumonia. About 15% of patients will need to be treated in hospital because of severe breathing difficulties. 5% will need the ICU and a ventilator. Patients who have recently completed or are undergoing cancer treatment are at higher risk of developing severe symptoms.
Based on the data available so far, the risk of death from COVID-19 in the general population is estimated by some models to be as high as 1%, which is 10x more fatal than the flu (about 0.1%). The real risk will only be known after widespread testing is available and we know how many people have been infected. Better knowledge of the disease process over time will likely also lead to improved, consistent treatment protocols that could also improve outcomes dramatically, and ultimately lower mortality to one that is more in line with the flu.
Most of the deaths have been in older patients with other medical conditions – the mortality rate for 60 – 64 year olds is about 4% for COVID-19. However, a significant number of younger people have also required admission to the hospital for supportive care. We are seeing deaths in all age groups, though younger, healthy people without other medical conditions appear to be at low risk for serious complications.
How do you protect yourself? Are there ways to reduce the risk of getting COVID-19?
Unfortunately, as of this post, there is currently no universally accepted treatment for Coronavirus. The anti-malarial drug hydroxychloroquine, either alone or in combination with azithromycin (Z-pack) and zinc, was initially reported as a potential “game-changer” treatment, but the data on whether this truly helps are mixed at best, and hydroxychloroquine can have significant side-effects. Several studies have actually cast serious doubt on the effectiveness of hydroxychloroquine for COVID-19. A recent study showed the antiviral drug Remdesivir can speed up recovery from a severe infection. However, for now, the best approach by far remains prevention.
People who recently completed or are currently in treatment for breast cancer are at higher risk for complications if they become infected. These recommendations will help protect you and reduce your risk of becoming infected:
- Social distancing – stay away from crowds and try to keep a distance of at least 6 feet between yourself and others when in public. The easiest way of avoiding the infection is to avoid people who are, or could be infected. Remember, many people who get infected won’t develop symptoms for several days. Cancel any non-essential doctor visits. If you can, please just stay at home.
- Wash your hands with soap and warm water for at least 20 seconds multiple times a day, especially after any contact with others. Use an alcohol-based hand sanitizer (containing at least 60% alcohol) when soap and water aren’t available.
- Avoid shaking peoples’ hands.
- Avoid touching your face, especially your eyes, nose and mouth.
- Clean and disinfect surfaces you touch daily, including household surfaces, the inside of your car, doorknobs, light switches, and your cellphone; make sure you use cleaning products that are effective in killing viruses.
- Politely tell friends and family who are sick to stay away from you.
- Make plans with your family or support structure in case you get sick.
- Ask your employer to work from home if at all possible.
- Fill your prescriptions and think ahead to make sure you’re not caught short with medications you need daily.
- Catch up on groceries and Make sure you have over-the counter medications like Tylenol in the house.
- Disinfect your groceries before putting them away, and wipe down or spray your mail and packages with disinfectant before bringing them into the house.
- Avoid unnecessary travel on public transport or airplanes.
- Avoid contact with people who have recently traveled to a highly impacted area.
- Postpone all non-essential doctors’ visits like routine follow ups.
- If you absolutely must leave the house, wear a cloth face mask over your nose and mouth, especially when going to stores or other areas where social distancing (6 ft) is difficult to maintain, or you will be in an enclosed area like a grocery store. You do not need to use a surgical face mask, so please do not hoard them. Our healthcare heroes on the front lines are in dire need of masks and other personal protective equipment.
What should you do if you develop symptoms?
If develop a fever, cough, or shortness of breath, please call your doctor. Most people with mild symptoms will be able to stay at home while the illness runs its course. However, if you develop symptoms you should definitely let your doctor know, by phone first before going in to see them.
If you develop a fever, don’t use ibuprofen – there is evidence that it may make this infection worse. Stick with Tylenol but be sure not to take more than the recommended dose.
What if you have surgery scheduled soon?
The decision to proceed with surgery will ultimately depend on several factors that need to balance the details of your diagnosis, the urgency of your surgery, travel requirements, and the protocols your team and hospital have in place. ‘Elective’ (non-urgent and non-emergent) surgeries have been on hold for many weeks now. Some facilities are now starting to allow elective procedures again, but this varies tremendously based on the geographic situation. It is very important for you to discuss this with your medical team. Learn more about the impact of COVID-19 on breast cancer treatment here.
This too shall ultimately pass!
Ultimately, we must keep reminding ourselves that this too shall pass. However, the above risk-reducing measures will not only protect you, but will also help decrease the spread of the virus. Social distancing is the best thing we can all do right now while we wait for a proven vaccine, and staying at home protects you and helps limit the spread of the virus as much as possible.
This is a constantly changing situation, so please be sure to check the CDC’s ongoing updates regularly.