Screening Mammograms Shown to Reduce Deaths Caused by Advanced Breast Cancer
There is a constant debate on whether screening mammograms offer a significant benefit to patients.

In the American Cancer Society journal, CANCER, a Swedish study has found that early mammogram screenings can significantly reduce the number of deaths from metastatic breast cancer.
The study evaluated 549,091 women, covering approximately 30% of the screening‐eligible population in Sweden. The results showed that women who had regular screening mammograms had a statistically significant 41% reduction in their risk of dying of breast cancer within 10 years, and a 25% reduction in the rate of advanced breast cancers, compared to individuals who did not participate in mammogram screenings. According to the study, these benefits appeared to be independent of recent changes in patient treatment regimens.
The study concludes that the “benefits of participating in mammography screening are truly substantial and save lives through early detection, lives that otherwise would have been lost under the prevailing therapy at the time of diagnosis.”
This study offers encouraging insight into the benefits of regular breast cancer screening. It is important for both women and men to discuss their overall risk of developing breast cancer to determine the best time to begin screening, and how often they should be screened.
Performing monthly at-home self-breast exams is also a very important, free screening tool everyone should practice in addition to regular radiologic screening. However, this should not replace the imaging screening recommended by your healthcare team.
If access to care or cost is keeping you from following through with your recommended breast cancer screening appointment, please check out the Financial Assistance tab within the Resource section in the Breast Advocate app.
Addressing Disparities between Black and White Women with Triple-Negative Breast Cancer
Multiple studies have shown that African-American women have poorer survival outcomes after a breast cancer diagnosis than white women. One significant contributing factor to these findings is that most studies include all types of breast cancer together. This approach can skew results as white patients have a higher incidence of estrogen receptor-positive breast cancer than black women, which has better outcomes than the more aggressive triple-negative form of the disease. A summary of the different types of breast cancer can be found here.
Survival rates between black and white women with triple-negative breast cancer (TNBC) appear to equalize when these cancers are found early with screening mammograms, a new JAMA study suggests. However, TNBC still remains about twice as common in black women.
This study emphasizes the importance of screening and early detection, particularly in traditionally underserved black women. Unfortunately, we still don’t know why black women experience a much higher rate of TNBC.

Supplemental MRI Screening May Benefit Women with Extremely Dense Breast Tissue
Women with extremely dense breast tissue have a 4 to 6 times increased risk of developing breast cancer, and their cancers are also less likely to be detected on a mammogram. About 50% of women have dense breasts.
New laws in many US states were recently passed requiring mammogram reports to include information on the density of a woman’s breast tissue. Dense breast tissue is a risk factor for breast cancer and can make detecting breast cancer more difficult with screening mammograms alone. For this reason, more research is underway to determine how to best screen for cancer in women with dense breasts.
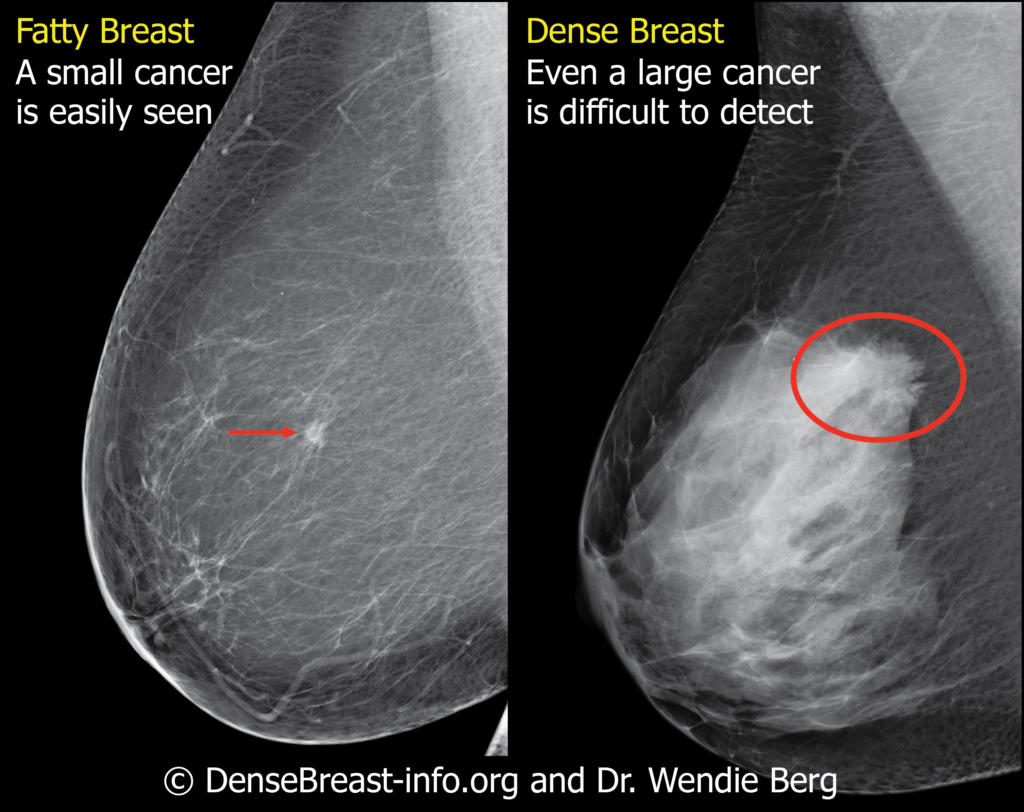
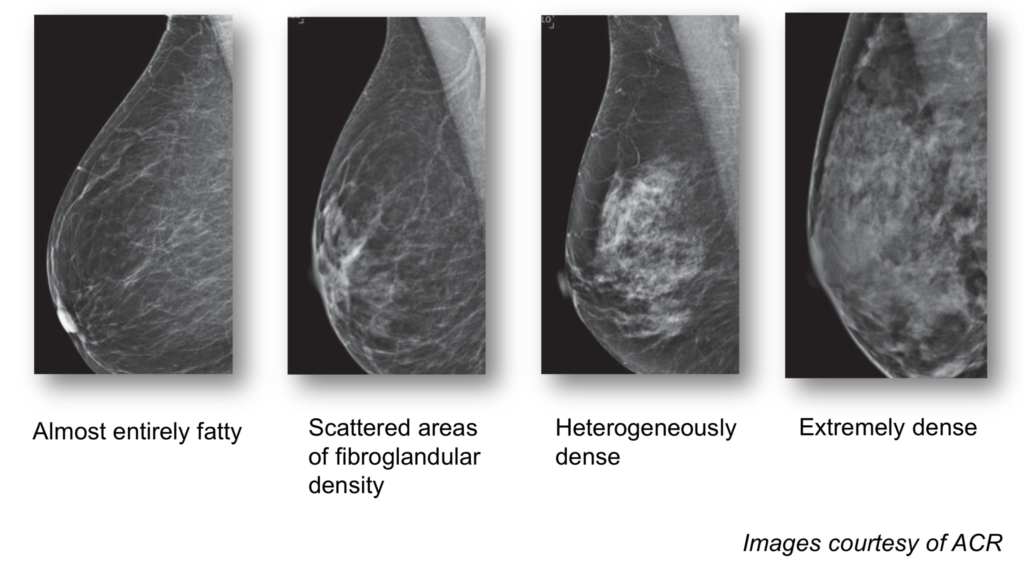
So what are “dense breasts”? Breasts consist of fibrous glandular tissue and fat. Dense breasts contain more fibrous tissue and less fat. On a mammogram, dense fibrous tissue has the same white appearance as a breast cancer. This can make it very difficult for radiologists to spot the breast cancer.
A long-standing question is whether or not women with dense breasts should undergo additional imaging screening tests in combination with mammograms. A new study published in the New England Journal of Medicine offers new insight supporting the addition of MRI screening to mammograms for women with extremely dense breast tissue.
The study was conducted in the Netherlands. 40,373 women between the ages of 50 and 75 years with extremely dense breasts and normal screening mammograms were randomized to undergo additional screening via MRI, or receive no additional screening. The study results showed the mammogram plus MRI group experienced 50% fewer interval cancers than the mammogram-only group during a 2-year period (2.5 vs 5 per 1,000 screenings, respectively). The tumors detected on MRI were smaller, of an earlier stage, and more likely to be node-negative than those detected in the mammography-only group.
This study suggests that a combination of mammograms and MRIs can be beneficial for women with extremely dense breast tissue in detecting breast cancer at an earlier stage than mammograms alone. However, it is important to note the results of this study do not suggest adding MRIs will decrease the death rates from breast cancer.
It is important to discuss your screening options with your health care team to see if additional MRI imaging would be beneficial for you based on your specific situation and risk of developing breast cancer.
Why you Need to Know Your Breast Density
A recently passed law means that for the first time in over 20 years, the FDA is updating regulations for mammography screening to give patients more information about their breasts. The amendments will specifically require that patients be informed of their breast density in all U.S. states.
Breast tissue that is more fatty in consistency appears dark gray or even black on a mammogram, which makes it fairly easy to identify a breast cancer since that appears as a white lesion on mammograms. Dense breast tissue consists mostly of glandular tissue and is not fatty at all. Glandular tissue also appears white on a mammogram making it harder to detect a cancer. Dense breasts can therefore mask a breast cancer.
Younger women are much more likely to have dense breasts than older women. As women approach menopause, the glandular tissue is gradually replaced by more fatty tissue.
About 50% of women in the U.S. have dense breasts. Women with the densest breasts are up to six times more likely to develop breast cancer than women with fatty breasts. Once diagnosed, a woman with dense breasts may have an increased chance of developing aggressive or metastatic breast cancer, which decreases her overall chance of survival.
The FDA will now require mammography centers and radiologists to share the patient’s breast density information on the mammogram report, in easy understandable language, along with how it might influence the accuracy of the mammogram. Women with dense breasts have additional screening options including 3D mammography, breast ultrasound, and MRI.
The new law is a major victory for the patient advocacy movement, in particular AreYouDense.org, founded by the late Nancy Capello, PhD. Dr Capello was responsible for the first state-based density reporting law passed in Connecticut in 2009 and spearheaded efforts to standardize the communication of dense breast tissue nationally through changes in the Mammography Quality Standards Act.
Large Number of Breast Cancer Survivors Not Getting Recommended Mammograms
Following a breast cancer diagnosis, women still need regular screening. However, a recent study shows many women are not following through with getting the recommended screenings they need.
The study followed over 27,000 women after their initial breast cancer surgery. The results showed one year after surgery, 13% of women had NOT had a mammogram. Over five years, only 50% of women had at least one mammogram each year.
The study also found that black women were less likely than white women to get an annual mammogram. “Lack of screening may contribute to higher death rates among black women, because recurrence of breast cancer is a major cause for poor outcomes in black women,” the researchers said.






